No need to wait for pandemics: The public health case for criminal justice reform
We offer five examples of policies that could slow the spread of a viral pandemic in prisons and jails - and would mitigate the everyday impact of incarceration on public health.
by Peter Wagner and Emily Widra, March 6, 2020
This briefing has been updated and expanded on March 27 with Five ways the criminal justice system could slow the pandemic. We recommend reading that one instead.
Since publishing this article, we have been tracking which prisons, jails and other criminal justice agencies are making meaningful policy changes to slow the spread of COVID-19. See our tracker, which we update daily, at https://www.prisonpolicy.org/virusresponse.html.
The United States incarcerates a greater share of its population than any other nation in the world, so it is urgent that policymakers think about how a viral pandemic would impact people in prisons, in jails, on probation, and on parole, and to take seriously the public health case for criminal justice reform.
Below, we offer five examples of common sense policies that could slow the spread of the virus. This is not an exhaustive list, but a first step for governors and other state-level leaders to engage today, to be followed by further much-needed changes tomorrow.
Quick action is necessary for two reasons: the justice-involved population disproportionately has health conditions that make them more vulnerable, and making policy changes requires staffing resources that will be unavailable if a pandemic hits.
The incarcerated and justice-involved populations contain a number of groups that may be particularly vulnerable to COVID-19, the novel coronavirus. Protecting vulnerable people would improve outcomes for them, reduce the burden on the health care system, protect essential correctional staff from illness, and slow the spread of the disease.
| Prevalence of health condition by population | ||||
|---|---|---|---|---|
| Health condition | Jails | State prisons | Federal prisons | United States |
| Ever tested positive for Tuberculosis | 2.5% | 6.0% | 0.5% | |
| Asthma | 20.1% | 14.9% | 10.2% | |
| Cigarette smoking | n/a | 64.7% | 45.2% | 21.2% |
| HIV positive | 1.3% | 1.3% | 0.4% | |
| High blood pressure/hypertension | 30.2% | 26.3% | 18.1% | |
| Diabetes/high blood sugar | 7.2% | 9.0% | 6.5% | |
| Heart-related problems | 10.4% | 9.8% | 2.9% | |
| Pregnancy | 5.0% | 4.0% | 3.0% | 3.9% |
The other reason to move quickly is that, on a good day, establishing and implementing new policies and practices is something that the government finds challenging to do on top of its other duties. If a pandemic hits and up to 40% of government lawyers are either sick or taking care of sick relatives and most of the rest are working from home, making policy change is going to be much harder and take far longer. If the government wants to protect both justice-involved people and their already overstretched justice system staff from getting the virus and spreading it further, they need to act now.
Here are five places to start:
- Release medically fragile and older adults. Jails and prisons house large numbers of people with chronic illnesses and complex medical needs, who are more vulnerable to becoming seriously ill and requiring more medical care with COVID-19. And the growing number of older adults in prisons are at higher risk for serious complications from a viral infection like COVID-19. Releasing these vulnerable groups from prison and jail will reduce the need to provide complex medical care or transfers to hospitals when staff will be stretched thin. (In Iran, where the virus has been spreading for several weeks longer than in the U.S., the government just gave temporary release to almost a quarter of their total prison population.)1
- Stop charging medical co-pays in prison. Most prison systems have a short-sighted policy that discourages sick people from seeking care: charging the free-world equivalent of hundreds of dollars in copays to see a doctor. In the context of COVID-19, not receiving immediate, appropriate medical care means allowing the virus to spread across a large number of people in a very confined space. These policies should all be repealed, but at a minimum should be immediately suspended until the threat of pandemic is over. (This will also reduce the administrative burden of processing and collecting these fees.)
- Lower jail admissions to reduce “jail churn.” About one-third of the people behind bars are in local jails, but because of the shorter length of stay in jails, more people churn through jails in a day than are admitted or released from state and federal prisons in 2 weeks. In Florida alone, more than 2,000 people are admitted and nearly as many are released from county jails each day.2 As we explained in a 2017 report, there are many ways for state leaders to reduce churn in local jails; for example, by: reclassifying misdemeanor offenses that do not threaten public safety into non-jailable offenses; using citations instead of arrests for all low-level crimes; and diverting as many people as possible people to community-based mental health and substance abuse treatment.3 State leaders should never forget that local jails are even less equipped to handle pandemics than state prisons, so it is even more important reduce the burden of a potential pandemic on jails.
- Reduce unnecessary parole and probation meetings. People deemed “low risk” should not be required to spend hours traveling to, traveling from, and waiting in administrative buildings for brief meetings with their parole or probation officers. Consider discharging people who no longer need supervision from the supervision rolls and allow as many people as possible to check in by telephone.
- Eliminate parole and probation revocations for technical violations. In 2016, approximately 60,000 people were returned to state prison (and a larger number were arrested), not because they were convicted of a new criminal offense, but because of a technical violation of probation and parole rules, such as breaking curfew or failing a drug test. States should cease locking people up for behaviors that, for people not on parole or probation, would not warrant incarceration. Reducing these unnecessary incarcerations would reduce the risk of transmitting a virus between the facilities and the community, and vice versa.
There is one more thing that every pandemic plan needs to include: a commitment to continue finding ways — once this potential pandemic ends — to minimize the number of confined people and to improve conditions for those who are incarcerated, both in anticipation of the next pandemic and in recognition of the every day public health impact of incarceration.
None of the ideas in this briefing are new. All five are well established criminal justice reforms that some jurisdictions are already partially implementing and many more are considering. These ideas are not even new to the world of pandemic planning, as we found some of them buried in brief mentions in the resources listed below — albeit after many pages about the distribution of face masks and other technical matters. Correctional systems need to be able to distribute face masks to the people who need them, of course, but making urgent policy decisions about changing how and where you confine people is not something that should be relegated to a sentence about how agencies may want to “consider implementing alternative strategies.”
The real question is whether the criminal justice system and the political system to which it is accountable are willing to make hard decisions in the face of this potential pandemic, in the face of the one that will eventually follow, and in the context of the many public health costs of our current system of extreme punishment and over-incarceration.
Appendix: Other resources for practitioners
While preparing this briefing, the Prison Policy Initiative identified some resources that may be helpful for facilities and systems that may be starting from scratch on a COVID-19 response plan, which we share below. This list is not intended to be comprehensive, and will hopefully soon be out of date as other agencies update and share their own plans:
- Correctional facilities pandemic influenza planning checklist, CDC, September 2007 (This checklist is very helpful, but many of the links in the document are broken as of this publication. Presumably the CDC will update this soon.)
- Pandemic influenza and jail facilities and populations, Laura Maruschak, et. al., American Journal of Public Health, September 2009
- Pandemic influenza preparedness and response planning: guidelines for community corrections, Patricia Bancroft, American Probation and Parole Association, August 2009
- How public health and prisons can partner for pandemic influenza preparedness: A report from Georgia, Anne C. Spaulding, et al., April 2009
Footnotes
-
Earlier this week, Iran reportedly released about 54,000 incarcerated people with sentences under five years, which is almost a quarter of their total prison population of 240,000 people, based on 2018 data from the World Prison Brief. ↩
-
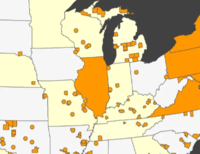
Although national numbers of jail releases per day are not available, the number of jail admissions — 10.6 million annually — is relatively stable, with the jail population turning over quickly, at an average rate of 54% each week. Assuming, then, that the number of admissions is about the same as the number of releases, we estimate that about 29,000 people are released from jails in the U.S. every day (10.6 million divided by 365 days per year). In comparison, in 2017, state and federal prisons admitted and released over 600,000 people, averaging about 12,000 releases a week or 1,700 per day. For state-by-state data, we estimated the number of releases in a similar fashion — we divided the number of annual admissions and releases, obtained from the Census of Jails, 2013, by 365 days. Governors of other states may want to see this table based on data from the Census of Jails, 2013:
State Jail Admissions Jail Releases Alabama 286,843 249,418 Alaska 5,392 3,686 Arizona 210,399 202,484 Arkansas 258,321 232,255 California 1,102,972 995,338 Colorado 211,397 197,866 District of Columbia 12,008 12,238 Florida 732,602 680,801 Georgia 602,648 537,857 Idaho 104,539 50,384 Illinois 315,553 290,264 Indiana 270,415 277,994 Iowa 127,179 123,693 Kansas 153,914 142,759 Kentucky 548,733 509,413 Louisiana 317,091 334,730 Maine 37,995 33,934 Maryland 156,659 164,736 Massachusetts 58,115 76,253 Michigan 359,631 348,584 Minnesota 188,662 180,393 Mississippi 125,961 119,682 Missouri 252,131 239,562 Montana 48,418 39,179 Nebraska 72,616 72,687 Nevada 144,256 146,657 New Hampshire 20,841 22,187 New Jersey 147,088 134,407 New Mexico 150,488 142,035 New York 219,320 201,939 North Carolina 417,199 433,700 North Dakota 39,367 35,979 Ohio 405,313 395,648 Oklahoma 409,293 261,454 Oregon 176,549 172,476 Pennsylvania 209,732 213,319 South Carolina 301,594 325,976 South Dakota 56,477 56,851 Tennessee 461,375 439,364 Texas 1,144,687 1,083,223 Utah 97,509 98,651 Virginia 355,549 304,466 Washington 283,627 305,963 West Virginia 47,439 46,210 Wisconsin 227,243 208,406 Wyoming 29,384 30,803 -
Policymakers should also double their efforts — without slowing down actual releases — to plan for a continuity of health care after release, including getting people signed up for Affordable Care Act coverage and giving them referrals for other treatment as needed. ↩



Prisons and jails should grant everyone 90-days of Good Time.
Most (if not all) jurisdictions have emergency authority to grant Good Time, and anyone within 90 days of release should not be controversial to release. Let people protect themselves, and reduce the strain on overpopulated institutions.
Finally, when prisons go to lockdowns, and don’t let families see each other and don’t all recreation or rehabilitation programs: People in cages should not be expected to peacefully sit still.