Compassionate release was never designed to release large numbers of people
With help from artist Kevin Pyle, we explain why very few people who apply for compassionate release are approved — even during a pandemic.
by Emily Widra and Wanda Bertram, May 29, 2020
With the coronavirus pandemic threatening to turn prison sentences into death sentences, many incarcerated people are seeking compassionate release — the release of people who are facing imminent death and who pose no threat to the public — to save them from dying of COVID-19 in prison. Unfortunately, what they, and the American public, are learning is that compassionate release is not a transparent and linear process, but an unpredictably ordered series of obstacles. As artist Kevin Pyle depicts here, these hurdles and delays kill the vast majority of compassionate release petitions:
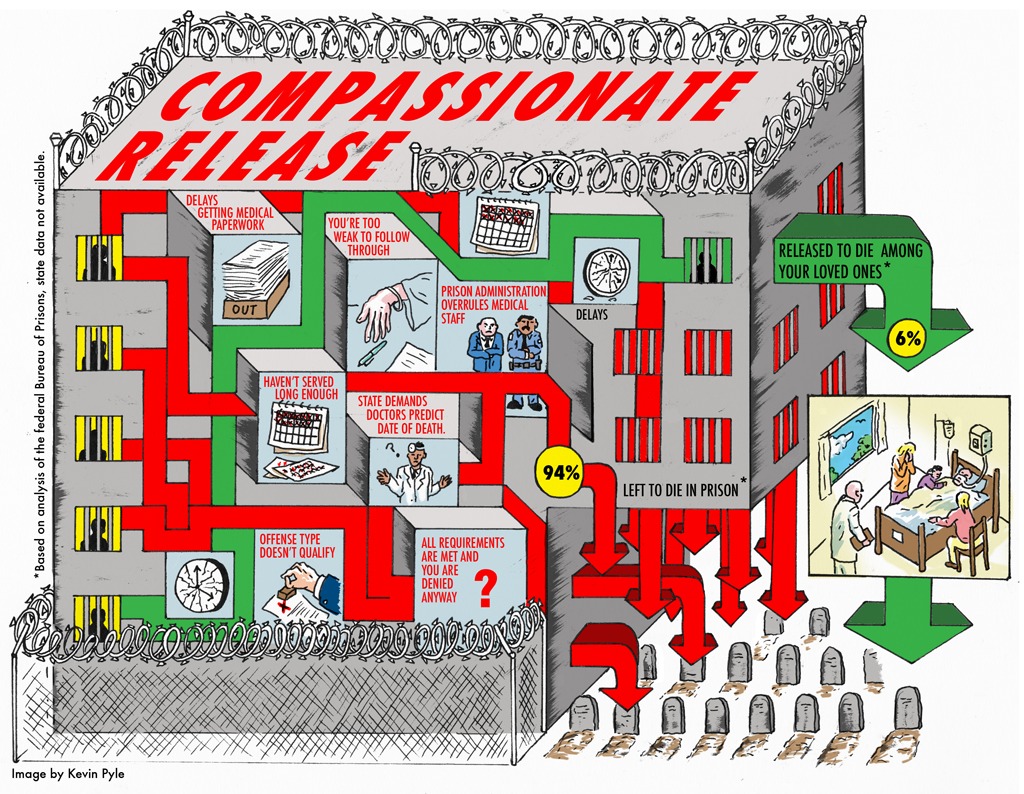
Applying for compassionate release is a lengthy and cumbersome process. Given that those who apply are almost always terminally ill or profoundly incapacitated, the arbitrary nature of this process means many die before their cases are resolved.1
The compassionate release process varies tremendously between states (some states even give it a different name, like “medical parole,” “geriatric parole”, etc.),2 but the basic framework is the same: An incarcerated person is recommended3 for release on compassionate grounds to prison administrators, who then solicit a medical recommendation, and then administrators or members of the parole board approve or deny compassionate release. Some states allow only family and attorneys to recommend that someone be released on these grounds; others allow incarcerated individuals to apply on their own behalf, or allow prison personnel to do so.
Compassionate release programs are plagued by many shortcomings, including:
- Requirements that a person be extremely close to death, or so incapacitated that they do not understand why they are being punished.4
- Requiring medical professionals to attest that someone is within six months, or nine months, of death. Health professionals are reluctant to give such exact prognoses, which means prison officials will default to saying “it’s safer just to not let this person go.”5
- Allowing the ultimate decision-makers6 to overrule recommendations from medical professionals and prison staff (e.g. by refuting or ignoring a medical prognosis).
The compassionate release process is frustratingly obscure not only for applicants, but for reporters, advocates, and others trying to understand the system. In their national survey, FAMM found that only three states are required to publish data on compassionate release grants, and eight other states publish some publicly available data, leaving most Americans in the dark about how often compassionate release is actually used. And despite that fact that FAMM has helpful memos for all fifty states and the District of Columbia detailing eligibility requirements for compassionate release, the application and referral process, the necessary documentation and assessments, and the decision-making criteria, the application process remains an arduous one.
There is plenty of room for states to improve their compassionate release processes. In our 2018 report Eight Keys to Mercy, we recommended that states:
- Make compassionate release available to all incarcerated people, irrespective of the offenses for which they are incarcerated.
- Streamline all compassionate release processes and set reachable deadlines so that petitioners don’t die due to bureaucratic bottlenecks before they are released.
- Limit the ability of prison officials to overrule, on medical grounds, a recommendation of release by medical professionals.
But even when a compassionate release system operates efficiently and fairly, the majority of people in prison are still not eligible for it. As currently constituted, these programs exclude too many people and these systems were never designed for quick responses during a global pandemic. States need to look beyond compassionate release — including expedited parole, and mass commutations — to slow the spread of the pandemic and prevent a needless tragedy behind bars.
Footnotes
- According to the New York Times, between 2013 and 2017, the federal Bureau of Prisons approved only 6% of the 5,400 compassionate release applications received; meanwhile, 266 other applicants died in prison. Their analysis of federal prison data shows that it takes over six months, on average, for an incarcerated person to receive an answer on their compassionate release application from the BOP. In one tragic example, prison officials denied an application for someone because the BOP put aside prison doctors’ prognosis of less than six months and concluded that he had more than 18 months to live, despite. Two days after receiving the denial, he died. ↩
- FAMM’s national survey found that not all states use the term “compassionate release” and instead refer to these programs as medical and geriatric parole, short- and long-term furloughs, suspension or reduction of sentences, and executive clemency on medical grounds. ↩
- There are major differences between state policies, but for a more comprehensive view of state policies, go to FAMM’s detailed breakdown on state practices in their 2018 report. ↩
- In Hawai’i, being “too ill or cognitively impaired to participate in rehabilitation and/or to be aware of punishment” can qualify someone for consideration for release on medical grounds. ↩
- In a uniquely positive development, new guidelines for federal prisons issued by the U.S. Sentencing Commission do not require a short-term “terminal” prognosis, as an excellent article in Health Affairs points out. ↩
- The “ultimate decision-makers” vary greatly by jurisdiction. For example, in the federal system, the prison warden makes a recommendation, but the final word on compassionate release comes from the Central Office of the Bureau of Prisons. In other jurisdictions, courts have the final say on compassionate release: in D.C., decisions are made in the superior court, and in Ohio the sentencing court rules on compassionate release. The Department of Corrections’ commissioner makes the decision in Massachusetts, Minnesota, and Mississippi (in Mississippi, the decision is made jointly with the Chief Medical Officer). In Arizona, Virginia, and West Virginia, the governor decides who is granted compassionate release after hearing a recommendation from the parole board. Many states rely on the parole board to make compassionate release decisions, including Alabama, California, and North Carolina. For the decision makers in every state, see FAMM’s state-specific memos. ↩