What do we know about the spread — and toll — of the coronavirus in state prisons?
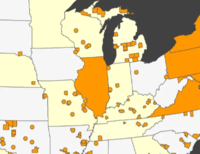
Wide variation in the rates of reported infections and deaths in state prisons reflect the uneven spread of the virus and disparate responses by state criminal justice systems.
by Emily Widra, June 24, 2020
We’re frequently asked about the number of infections and deaths in prisons from the coronavirus that causes COVID-19. The UCLA COVID-19 Behind Bars Data Project is helpfully collecting all of the official reports of infections and deaths into a single Google Sheet. But state prison systems are vastly different sizes, so it’s impossible to make direct comparisons using only the counts provided in the UCLA spreadsheet. So we’ve calculated the rates of infection and deaths in state prison systems, which allow us to compare the impact of the pandemic across all 50 states’ prison populations. Our findings, presented in the table below, suggest three possible – and troubling – conclusions:
- Some states may not be properly testing or may not be accurately reporting infections and deaths;
- People incarcerated in different states may face very different odds of infection and death from COVID-19, depending on how their state responds to the crisis; and/or
- Some states have been lucky in that the virus has been slow to reach their facilities. But, as we’ve seen with the uneven spread of the pandemic across states, this likely means the full force of the virus has yet to hit these facilities, so they need to redouble their efforts at population reduction and other preparations.
Number and rate of COVID-19 deaths, cases, and tests in state prisons
| State | COVID deaths in prisons | COVID confirmed cases in prisons | Number of tests given | Prison population | Deaths per 10,000 incarcerated people | Infections per 10,000 incarcerated people | Deaths per confirmed case (“case fatality rate”) |
|---|---|---|---|---|---|---|---|
| Alabama | 4 | 41 | – | 27,164 | 1.47 | 15.09 | 9.8% |
| Alaska | 0 | 2 | 717 | 3,985 | 0 | 5.02 | 0% |
| Arizona | 7 | 252 | 3,005 | 41,386 | 1.69 | 60.89 | 2.8% |
| Arkansas | 5 | 1,277 | – | 17,331 | 2.89 | 736.83 | 0.4% |
| California | 17 | 3,215 | – | 119,327 | 1.42 | 269.43 | 0.5% |
| Colorado | 3 | 627 | – | 18,419 | 1.63 | 340.41 | 0.5% |
| Connecticut | 7 | 871 | – | 10,973 | 6.38 | 793.77 | 0.8% |
| Delaware | 0 | 148 | – | 5,081 | 0 | 291.28 | 0% |
| Florida | 18 | 1,665 | – | 92,574 | 1.94 | 179.86 | 1.1% |
| Georgia | 20 | 496 | – | 53,648 | 3.73 | 92.45 | 4.0% |
| Hawai’i | – | 0 | 16 | 4,260 | 0 | 0 | – |
| Idaho | 0 | 0 | 62 | 9,028 | 0 | 0 | – |
| Illinois | – | 256 | – | 37,731 | 0 | 67.85 | – |
| Indiana | 19 | 697 | 1,798 | 26,707 | 7.11 | 260.98 | 2.7% |
| Iowa | – | 30 | 2,068 | 8,899 | 0 | 33.71 | – |
| Kansas | 4 | 894 | – | 9,740 | 4.11 | 917.86 | 0.4% |
| Kentucky | 2 | 366 | – | 21,397 | 0.93 | 171.05 | 0.5% |
| Louisiana | 15 | 614 | – | 29,682 | 5.05 | 206.86 | 2.4% |
| Maine | 0 | 4 | 982 | 2,123 | 0 | 18.84 | 0% |
| Maryland | 7 | 357 | 32,848 | 18,686 | 3.75 | 3.75 | 2.0% |
| Massachusetts | 7 | 416 | 6,958 | 7,778 | 9.00 | 534.84 | 1.7% |
| Michigan | 68 | 3,981 | 38,191 | 36,980 | 18.39 | 1,076.53 | 1.7% |
| Minnesota | 0 | 290 | – | 8,457 | 0 | 342.91 | 0% |
| Mississippi | 2 | 34 | – | 18,553 | 1.08 | 18.33 | 5.9% |
| Missouri | 1 | 52 | – | 25,133 | 0.40 | 20.69 | 1.9% |
| Montana | 1 | 2 | 760 | 2,674 | 3.74 | 7.48 | 50.0% |
| Nebraska | 0 | 7 | – | 5,537 | 0 | 12.64 | 0% |
| Nevada | 1 | 7 | – | 12,127 | 0.82 | 5.77 | 14.3% |
| New Hampshire | – | 1 | 33 | 2,513 | 0 | 3.98 | – |
| New Jersey | 46 | 2,518 | – | 17,519 | 26.26 | 1,437.30 | 1.8% |
| New Mexico | 1 | 117 | – | 6,558 | 1.52 | 178.41 | 0.9% |
| New York | 16 | 516 | – | 40,956 | 3.91 | 125.99 | 3.1% |
| North Carolina | 5 | 713 | 3,451 | 32,795 | 1.52 | 217.41 | 0.7% |
| North Dakota | 0 | 5 | – | 1,461 | 0 | 34.22 | 0% |
| Ohio | 79 | 4,513 | 13,197 | 48,453 | 16.30 | 931.42 | 1.8% |
| Oklahoma | 0 | 1 | 2,544 | 24,947 | 0 | 0.40 | 0% |
| Oregon | 1 | 168 | 670 | 14,355 | 0.70 | 117.03 | 0.6% |
| Pennsylvania | 9 | 262 | – | 43,852 | 2.05 | 59.75 | 3.4% |
| Rhode Island | 0 | 48 | – | 2,395 | 0 | 200.42 | 0% |
| South Carolina | – | 108 | – | 18,160 | 0 | 59.47 | – |
| South Dakota | 0 | 4 | – | 3,679 | 0 | 10.87 | 0% |
| Tennessee | 4 | 3,141 | 23,091 | 27,946 | 1.43 | 1,123.95 | 0.1% |
| Texas | 54 | 7,445 | – | 151,126 | 3.57 | 492.64 | 0.7% |
| Utah | 0 | 14 | 315 | 6,064 | 0 | 23.09 | 0% |
| Vermont | 0 | 48 | – | 1,369 | 0 | 350.62 | 0% |
| Virginia | 9 | 1,328 | – | 28,595 | 3.15 | 464.42 | 0.7% |
| Washington | – | 108 | – | 16,531 | 0 | 65.33 | – |
| West Virginia | 0 | 124 | – | 6,550 | 0 | 189.31 | 0% |
| Wisconsin | – | 264 | 12,779 | 22,681 | 0 | 116.40 | – |
| Wyoming | 0 | 0 | – | 2,465 | 0 | 0 | – |
An important disclaimer: It would be a mistake to use this table as an indication of “how good a job” any state has done in responding to the threat of the pandemic behind bars. No state has even come close to adequately protecting its incarcerated people. Certainly, some states have done more than others to release more medically vulnerable people, and some states’ correctional healthcare systems are less terrible than others, which may increase the odds of surviving COVID-19 in some prisons. We also acknowledge that some states have taken small steps to reduce the population density of their facilities; still, none have done so on a scale that would make social distancing possible or otherwise slow the spread of the virus.
We are skeptical of the officially reported data for several reasons, but especially because of the wide variation in the “case-fatality rates” – that is, the number of deaths relative to the number of infections reported by each state. Why does Tennessee report 785 infections for every death and Alabama reports 10 infections for every death? Both states have similarly-sized prison populations and both states report 4 confirmed COVID-19 deaths among incarcerated people. But it would appear that Tennessee is doing a lot of testing and Alabama is not.
Comprehensive and frequent testing offers the prison system – and the public – a clearer view of the virus spread. If correctional facilities are only testing people with extreme symptoms, we gain very little information about what to expect and how to protect vulnerable lives.
The number of reported deaths may also reflect undercounts for other reasons. For example, unless a state tests everyone who dies in custody, it is likely excluding a number of deaths that were caused by COVID-19 but were not confirmed by testing. Especially where states are severely under-testing, people will be dying of COVID-19 but left out of the official death counts because they were never tested. Similarly, it would be appropriate to classify people who “recover” from COVID-19, but remain weakened and then die of another cause, as COVID-19 deaths. We have not heard of any state prison systems that are counting deaths other than those confirmed by tests, however.
The data, imperfect as it is, tells us that people incarcerated in different states may face vastly different odds of infection and death from COVID-19. The inaction of state prison systems is unconscionable given that, for months, the largest outbreaks of the coronavirus have been in correctional facilities. States put their residents at grave risk by failing to prevent the spread of the virus in the “petri dishes” that are prisons and jails. They should be using every tool available to ramp up efforts to protect incarcerated people, which includes widespread testing and using testing data to target resources to the people and places most at risk.
Table sources
- COVID deaths in prisons: UCLA Law School’s Covid-19 Behind Bars Data Project
- COVID confirmed cases in prisons: UCLA Law School’s Covid-19 Behind Bars Data Project
- Number of tests given: Covid Prison Data Table 2, as of June 19, 2020
- Prison population: Vera Institute of Justice’s People in Prison 2019, supplemented by correspondence between the Prison Policy Initiative and individual state Departments of Correction. All population counts are from May 2020 except for Maryland’s, which is from December 31, 2019.
- Deaths per 10,000 incarcerated people: Calculated by dividing the number of COVID deaths by the prison population, then multiplying by 10,000
- Infections per 10,000 incarcerated people: Calculated by dividing the number of COVID cases by the prison population, then multiplying by 10,000
- Deaths per confirmed case (“case fatality rate”): Calculated by dividing the number of deaths by the number of COVID cases, then multiplying by 100. For more information about case fatality rates and factors that affect the accuracy of these rates, see this New York Times article. The wide variation seen in the prison data suggests that these rates may reflect differences in testing more than differences in severity or treatment of the disease across different states.