Lessons from COVID-19 can help prisons & jails prepare for the next pandemic
COVID-19 wasn’t the first virus to devastate prisons and jails…and it won’t be the last. By learning from their past failures, state and local leaders can take steps now to prepare for the next inevitable viral threat.
by Emily Widra, April 21, 2023
On Monday, April 10th, President Biden signed a congressional resolution ending the national emergency declaration, and the separate national public health emergency declaration is set to expire on May 11th, thereby rolling back the last major federal policies designed to respond to the ongoing threat of COVID-19. As the nation enters this new period, we reviewed the experience of COVID-19 — and other pandemics and epidemics behind bars — to understand what correctional institutions and policymakers need to do to prepare for when the next viral outbreak occurs.
A pattern of pandemics and epidemics behind bars
COVID-19 wreaked havoc on the nation’s jails and prisons, with more than 3,000 deaths among incarcerated people, 300 deaths among correctional staff, 660,000 reported cases among incarcerated people, and 247,000 reported cases among correctional staff. The pandemic underscored what public health experts have long known: prisons and jails are not designed to provide adequate health care or prevent disease transmission, and in fact, they often are the sites of disease outbreaks.
It is important to recognize, though, the terrible consequences of the COVID-19 pandemic behind bars weren’t necessarily unique to this particular virus. Rather, COVID-19 is one more example of a historic pattern of just how vulnerable people in jails and prisons are to communicable illnesses and how — without any serious change to our reliance on mass incarceration — this population will continue to bear the disproportionate burden of public health crises, inevitably affecting the health of communities outside of correctional facilities as well.
Tuberculosis
The tuberculosis (TB) pandemic is primarily concentrated outside of the United States, but people in prisons and jails within the U.S. are disproportionately affected by TB when compared with the general U.S. population. TB cases and diagnoses have decreased steadily since 1992 in the U.S., but rates of TB in local jails, state prisons, and federal prisons actually increased from 2020 to 2021.
Hepatitis
Hepatitis C — considered an epidemic — is also significantly more common among incarcerated populations than the general U.S. population: in 2012, 11% of people in state and federal prisons had ever been diagnosed with Hepatitis B or C, compared to only 1.1% of the general U.S. population.1 While the virus is generally considered treatable outside the walls of a prison, state and local leaders have consistently missed the opportunity to get control of the virus behind bars by their failure to implement screening and treatment protocols behind bars.
HIV/AIDS
An estimated one in seven individuals living with HIV passes through the correctional system annually. Nationally, the overall prevalence rate of HIV in the U.S. in 2019 was 431 per 100,000 people and the number of new HIV infections declined 8% from 2015 to 2019. But HIV/AIDS is far more prevalent in prisons. The total U.S. prison population faces an prevalence rate that is more than 2.5 times higher: 1,144 per 100,000 people in prison have HIV/AIDS, highlighting how disproportionately affected incarcerated people are by HIV.
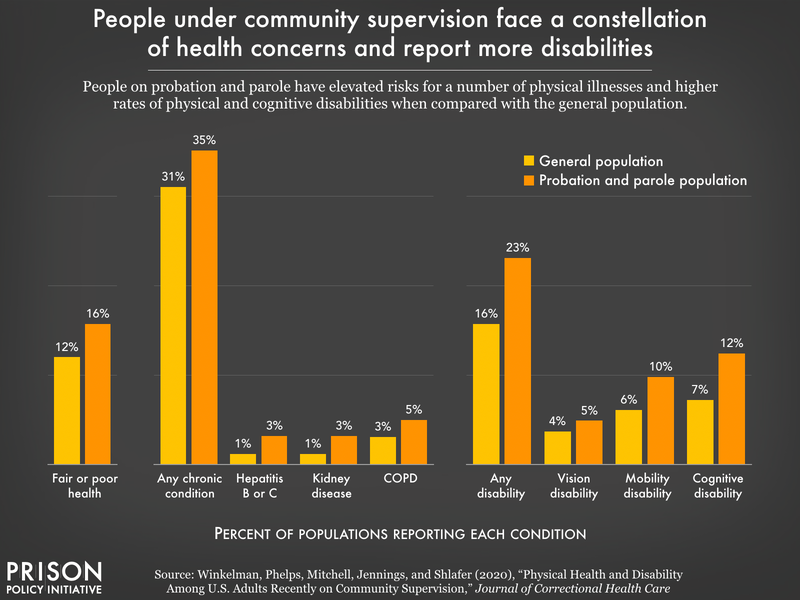
What these disease-specific disparities show is simple: for so many illnesses and diseases, incarcerated people face higher rates of infection and illness than their non-incarcerated counterparts.
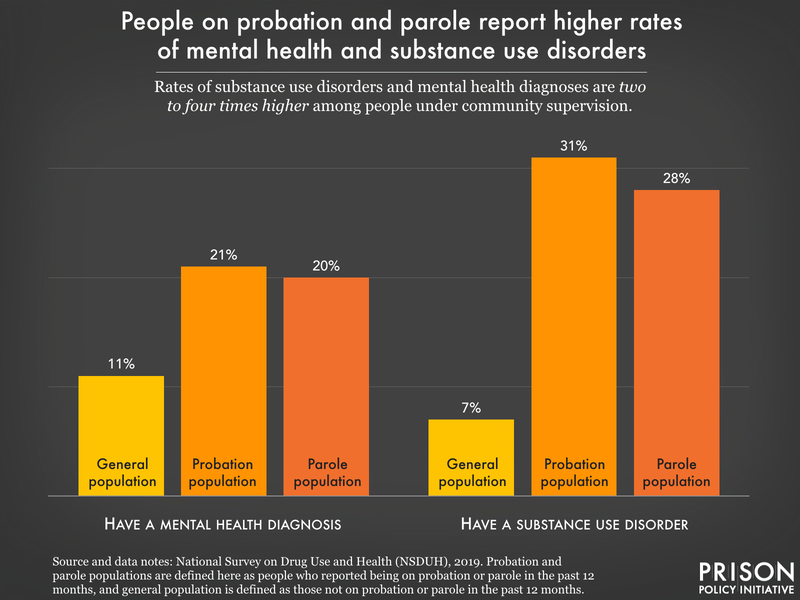
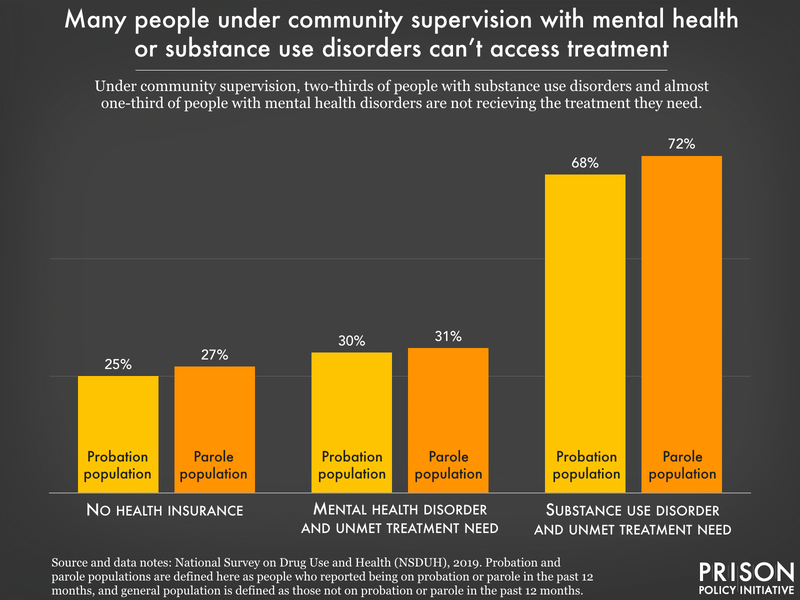
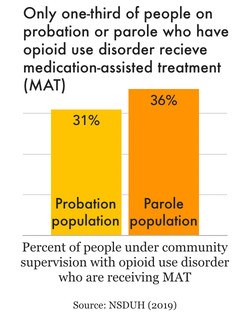
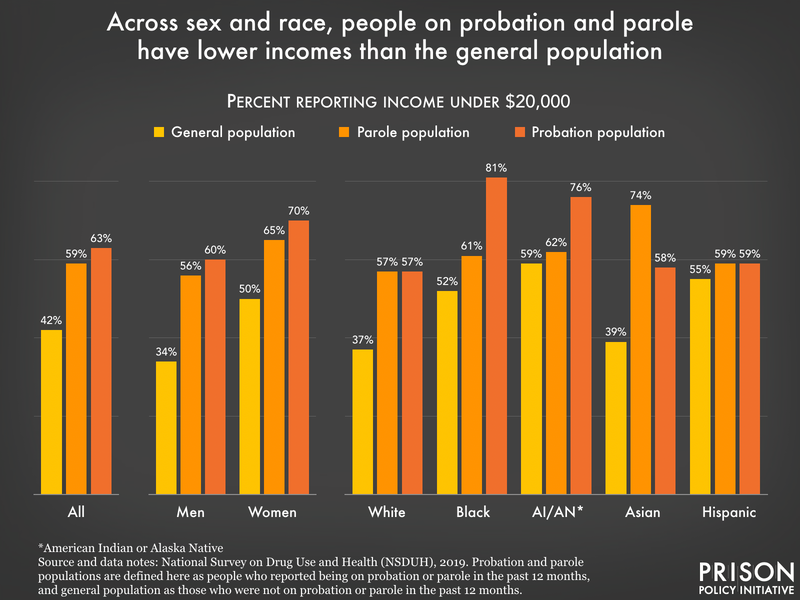
The elevated rates of infection and disease are correlated with a number of other factors that overlap significantly in the incarcerated population, including poverty, lack of access to healthcare and insurance prior to incarceration, homelessness, history of drug use and other preexisting chronic health issues, inadequate correctional health care, congregate living settings of correctional facilities, and health care gaps upon release from prisons and jails. So, regardless of what the next pandemic brings, we know that people in prisons and jails are particularly vulnerable to communicable diseases and often face higher mortality rates than those outside of prison walls facing the same illness.
Lessons learned
To even begin to prevent catastrophic illness and death behind bars during the next inevitable outbreak, correctional institutions and policymakers need to reflect on the emergency (and preparatory) measures that COVID-19 showed were necessary.
Reduce incarcerated populations:
In prisons:
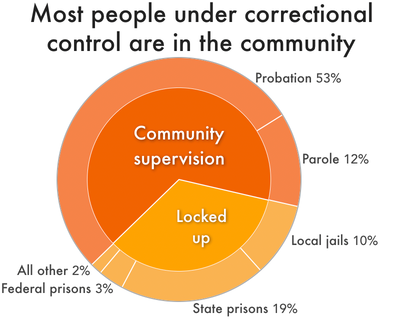
- Departments of corrections should not incarcerate people for technical violations of probation and parole rules. In 2016, 60,000 people were returned to state prison for behaviors that, for someone not on probation or parole, would not be a crime.
- Departments of corrections and state officials should expand the use of “good time” credits, and expand the use of clemency and commutations. Parole boards need to hold more — not fewer — hearings to let more people go home.
In jails:
- State and local legislatures can expand the list of “non-jailable” offenses, which are not subject to arrest but can only be fined or cited.
- Police and law enforcement departments can reduce the number of arrests — especially for “petty offenses” — and prosecutors can opt out of prosecuting people for certain offenses utilizing diversion services or other alternatives to incarceration.
- Jails can refuse to rent space to other agencies. In some states, as much as 8% of jail capacity is dedicated to USMS, 10% to ICE, and 66% to state prisons.
- Jails should refuse to admit people accused of violating technical rules of their state probation or parole. As we recently found, people detained for technical violations can make up a huge part of a jail’s population.
- Nobody should be detained simply because they cannot afford money bail.
Improve health services during incarceration:
- Eliminate medical co-pays. Unaffordable medical copays in prisons and jails can lead to increased spread of disease in and around correctional facilities and postpone access to medical treatment, often resulting in worsening ailments/illnesses. With a highly infectious virus posing an ongoing threat, this can have deadly consequences. Forty states still charge incarcerated people copays to seek medical treatment. While some states suspended these fees during the COVID-19 pandemic, many have already reinstated them.
- Support access to existing vaccines and promote vaccine education. Vaccination efforts should include an educational component that allows incarcerated people to get the information necessary to feel comfortable taking the vaccines. Additionally, the relationship between people in prisons and the medical staff of that prison is often defined by mistrust. Information about the safety and efficacy of any vaccine is limited for people behind bars, and governments should bring in outside medical experts and community leaders who will have the trust of the people who are incarcerated and give them multiple opportunities to ask questions and voice their concerns.
Develop systems to identify and respond to viral outbreaks early:
- Establish metrics to identify outbreaks and protocols to respond to them: Corrections officials must recognize that the threat posed by viral outbreaks could dramatically increase quickly. They should have established processes to monitor the threat the virus poses and, when appropriate, plans to impose more rigorous interventions — such as education, masking, increased testing, and enhanced hygiene practices — to stop its spread.
- Create outbreak response plans. During the COVID-19 pandemic, rather than developing plans to mitigate the harm of an inevitable outbreak, most states were focused on restricting the movements of incarcerated people within facilities — in other words, they attempted to “contain” the virus, which is all but impossible with communicable diseases. While many facilities do have outbreak plans for specific illnesses (like influenza), these plans are often outdated. Such plans should be reviewed and updated frequently, and should always include up-to-date contacts in local public health departments.
- Include incarcerated populations in the priority groups for testing, treatment, and vaccinations.
Conclusion
Our colleagues at the UCLA Law COVID Behind Bars Data Project found that the mortality rate in U.S. prisons increased by 61% during the first year of the pandemic. There is no doubt that the failure of officials across the country to quickly and adequately respond to the COVID-19 pandemic in correctional settings is to blame. Moving forward, prisons and jails need to remember the lessons learned during the past three years to avoid repeating the same mistakes that helped the virus spread within both prisons and the surrounding communities. The nation’s overreliance on incarceration has left too many vulnerable people behind bars in the face of public health crises.
Footnotes
-
We use 2012 data here because the Bureau of Justice Statistics’ report, Medical Problems of State and Federal Prisoners and Jail Inmates, 2011-12, contains a general population estimate that is standardized to match the prison population by sex, age, race, and Hispanic origin for 2012. In 2016, 10% of people in state prisons and 4% of people in federal prisons reported ever having hepatitis, but there is no standardized general population comparison included in that report. ↩