How prepared are state prison systems for a viral pandemic?
We sent state prison systems a 5-question survey, and the answers – largely – are not encouraging.
by Emily Widra and Peter Wagner, April 10, 2020
Many local jails and pretrial systems are taking action to reduce their populations in advance of the COVID-19 pandemic, but state prison systems are not, raising the question: Are state prisons prepared to handle a pandemic within their walls? We set out to survey prison systems on the capacity of their health facilities, their plans for any necessary external hospitalizations, their levels of equipment, their staffing levels and their general priorities.
Unfortunately, our April 3-10 survey shows that state prisons are still largely unprepared for a global pandemic that can reasonably be expected to hit their entire state prison system — and their supporting state government — all at the same time.
Most prisons are still aiming to keep the virus out of their facilities, rather than focusing on how to minimize the harm to incarcerated people, to their staff and to society as a whole. Containment might be a reasonable goal when it comes to outbreaks of flu, tuberculosis, or MRSA – diseases that prison systems know how to guard against by vaccinating people, screening, and so on. But COVID-19 is different both in terms of how it spreads and by the fact that it is already stressing the public hospital system that state prisons historically rely on for back-up support.
Given the number of large number of staff required to run a facility1 and the apparent ease with which asymptomatic people can infect others, no combination of security restrictions — such as suspending family visitation, checking the temperature of incoming staff, or confining the entire population to their cells — can keep out the virus that causes COVID-19 for long.2 And once the virus enters a facility, the density and lack of sanitation will allow it to spread quickly to all incarcerated people and staff, and will accelerate the spread to the surrounding community.
Ideally, state prisons’ first response to the pandemic should have been to do like many jails and reduce the number of people incarcerated. But at the very least, we expected to see them developing plans that acknowledged the inevitability of a COVID-19 outbreak and its unique challenges. Their plans should anticipate the need to isolate vulnerable people, work around staffing shortages, and navigate shortages of medical supplies and hospital beds. But except for a few notable exceptions — particularly North Dakota — most states have not even gotten that far.
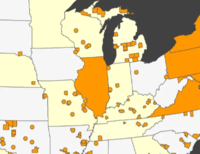
The good news is that in some states, the spread of the virus is several weeks behind other states, so some of the states that are the least ready still have the potential to learn from other states and improve their planning.
The state of pandemic planning in state prisons
In our survey of state Departments of Corrections, we sought to gather more information about how states are preparing for the pandemic to breach the prison gates. We asked about five major topics of pandemic preparedness:
- the capacity for isolating particularly vulnerable individuals and quarantining people with suspected cases of COVID-19 within facilities,
- protocols for people requiring hospitalization,
- equipment (including ventilators, medical-grade PPE, COVID-19 tests) accessible to facilities,
- anticipated staffing changes and availability of healthcare staff within facilities, and
- what the most immediate priorities are in planning for a COVID-19 outbreak in correctional facilities.
You can read the individual responses, but let’s jump to what the answers should have been.
We hoped to hear from each state that steps were being taken to prepare facilities to navigate the inevitable: a positive COVID-19 test among the hundreds of people living in close proximity to one another in prison. We expected each facility to have designated cells, units, or wings that could be easily isolated from the rest of the facility to allow either isolation of people who are particularly vulnerable to complications from COVID-19, or quarantine of people who test positive for COVID-19.
Given the recommendation from expert Dr. Homer Venters that facilities establish a plan for hospitalizations that recognizes that staff will be in short supply, and thus does not require the usual 2:1 ratio of correctional officers to patients, we expected correctional departments to have established new pathways and protocols for hospitalization.
We also expected that because prisons have finite resources for respiratory support (such as oxygen), facilities would have realistic plans to transfer people to hospitals while protecting staff from exposure. We hoped prisons could tell us how they would secure sufficient equipment and supplies, and how they will respond when supplies run out or when hospitals refuse to admit. (For example, there is already a shortage of COVID-19 tests, restrictions on who can be tested, and personal protective equipment (PPE) for medical professionals is already in short supply.) This planning, unfortunately, was largely absent.
Given the rate of infection and the length of hospitalization for severe cases of COVID-19, it is reasonable to assume facilities will encounter staffing shortages and that plans need to be in place for making sure the essential services behind bars continue in the face of staff calling out sick (i.e. food, medical care, telephone access, etc.). Given that most correctional staff are already stretched thin, departments should have begun planning for a staffing shortage weeks ago by reducing the number of people incarcerated and reducing the burden on staff. Most departments did not, but we still expected that they were preparing for the medical challenge created by that inaction.
The responses we received were largely disappointing. Rather than developing plans to mitigate the harm of an inevitable outbreak, most states are still focusing on restricting the movements of incarcerated people within facilities — in other words, attempting to “contain” the virus, which is all but impossible with COVID-19.
Even worse, some state departments of corrections informed us that no changes to their existing medical capacity were needed, suggesting that their established medical facilities and staff were sufficient to combat a disease that is overwhelming entire city infrastructures across the nation. Other states notified us that because no positive cases had occurred in their prisons, many changes have not yet been implemented. A number of states referred us back to their websites, which although providing up-to-date information on some aspects of their COVID-19 response, did not answer the specific questions about policy and planning changes in the past few weeks.
The good news is that many states still have time to do a far better job. At this point, on April 10, state Departments of Corrections need to be focused on mitigating the disastrous consequences of the COVID-19 pandemic entering prisons, rather than sticking to the belief that their high prison walls can effectively keep a global virus at bay.
Footnotes
-
Every facility is different, but outside observers can roughly estimate the number of staff that go in and out of a facility by dividing the incarcerated population by 4.6 for jails and 4.7 for prisons. (The typical jail has one staff member for every 3.3 incarcerated people, and the typical prison has one staff member for every 3.4 incarcerated people. If you assume that the staff work 5 days out of 7, you can divide the incarcerated population by 4.6 or 4.7 to get an estimate of how many staff enter and leave the facility every 24 hours.)
The initial incarcerated to staff ratios of 3.3 and 3.4 were calculated from the Bureau of Justice Statistics’ Jail Inmates in 2018 and Census Of State And Federal Correctional Facilities, 2005, Appendix Table 14. ↩
-
We are separately tracking press releases and updates from state departments of corrections on visitation suspension, changes in communication costs, screening policies for staff and new admissions, and facility lockdowns.
↩



In Connecticut we had pleaded with our governor early in the crisis to consider expedited releases of those toward the end of their sentence and pose no threat to public safety , We have wrote letters, made calls, requested zoom meetings to be rejected, used twitter account messaging and Facebook messaging to appeal to the governor. He flat out refused to consider early release from day one and has only now after numerous public protests begun to make tiny steps toward releasing those who had been approved before the pandemic which accounts to approximately 80 people. The only plan he and the Commissioner of Corrections put in place was to send anyone with symptoms to Northern control unit which advocates had been pushing to shut down for the past 2 years due to the inhumane treatment that occurs inside. The United Nations Special Rapporteur on Torture had supported our movement stating the facility practices may be considered torture according to International Law. Hundreds have been sent there since the virus is ravishing all the prisons and many more fear admitting they are sick knowing transfer to the control unit on 24 hour lockdown is the administration’s only response to this health crisis. The struggle continues because the message advocates and families are hearing is the lives of the incarcerated are disposable. One man died a week ago. A man who had been previously approved for release on a 2 year sentence. His sentence in effect became a death sentence due to the indifference shown the incarcerated.