Cut-rate care: The systemic problems shaping 'healthcare' behind bars
In correctional healthcare systems, care is secondary to controlling costs and avoiding lawsuits — a problem plaguing both private and public healthcare delivery. What will it take to get people the care they need?
By Brian Nam-Sonenstein
February 2025
Press release
- Table of Contents
- What’s driving correctional healthcare policy?
- Cost control
- Shielding from lawsuits
- Public care vs. Private care
- Correctional healthcare “accountability”
- Corrections oversight
- Accreditation
- Litigation
- Recommendations
- Shift the incentives
- Higher standard of care
- Appendix: Correctional healthcare history
- Footnotes
- What’s driving correctional healthcare policy?
- Cost Control
- Shielding from lawsuits
- Public care vs. Private care
- Correctional healthcare “accountability”
- Corrections oversight
- Accreditation
- Litigation
- Recommendations
- Shift the incentives
- Higher standard of care
- Appendix: A history of correctional healthcare
While people in the United States have long struggled with cost, quality, and access to healthcare, the crisis is particularly severe for people confined in jails and prisons. Since 2000, conditions have been so bad that roughly half of all state prison systems have been court-ordered to improve mental and medical healthcare,1 according to our analysis of data from The Civil Rights Litigation Clearinghouse. Alabama prisons have been hit with six healthcare-related court orders in that time — more than any other state — followed by California (5) and Colorado, Connecticut, New York, and Wisconsin (3 each). These court orders cover a wide range of healthcare issues, including insufficient policies, understaffing, failure to provide medication and treatments, and lack of quality monitoring and reporting; they paint a frightening picture of the scale of the problem facing incarcerated people. But lawsuits are an extremely limited metric by which to judge the quality of correctional healthcare: it’s very difficult for incarcerated people to successfully sue over their conditions, and many people endure medical neglect and abuse that never makes it before a judge. In other words, the reality is almost certainly worse.

It’s no secret that incarcerated people are routinely failed by their healthcare providers. Every year, dozens of news articles and broadcasts, government audits, and advocacy groups spotlight healthcare issues in federal, state, and local lock-ups. Yet, the quality of healthcare in jails and prisons remains poor: health issues and mortality rates remain at crisis levels, costs continue to mount, and departments cycle through contracts with various medical providers in just a few short years. Meanwhile, prisons routinely fail to meet the healthcare and treatment needs of incarcerated people. To make matters worse, corrections facilities are designed and operated in ways that actually worsen the health of incarcerated people. Many features of incarceration make symptoms of mental illness worse and aid in the spread of infectious disease. Prisons are also environmental hazards that have serious consequences for the health of people who live in and around them.
What needs to change for incarcerated people to get the healthcare they need? For this report, we pored over research, news investigations, government reports, and contractor documents to better understand the “big picture” relationship between healthcare providers, government agencies, and incarcerated people, and to identify system-level targets for improving care outcomes. Since so much analysis overlooks the experiences of incarcerated people, we also turned to dozens of people inside for their input. You’ll find their perspectives2 throughout this report in boxes, like this one:
Prior to prison I had wonderful medical care, and caring, helpful, professional [medical staff who] certainly listened to my issues, sufferings, and medical needs. I was given respect, time to speak, and serious treatment based on helping me, not just trying to shut me up and get me out of their office. The priorities and the approach were to help me, to try and make my condition manageable so I wasn’t suffering.
My access to medical treatment here in prison is fake. It’s not real and every problem is fixed with Naproxen and a bandaid. I am disabled. I am denied medical help. I am denied my medications I was on when taken into custody of the federal government — forced to detox and suffer daily, treated like my conditions are fake, phony, or unimportant. My medical doctors, nurses, and staff from [University of Pittsburgh Medical Center] [and counselors were] amazing before I was taken into the [Bureau of Prisons] system.
— John N.
Ultimately, we find that “correctional healthcare” is not really healthcare in the traditional sense when one looks at the business model and who it serves. Correctional healthcare systems are designed in such a way that incarcerated people’s health needs are treated more like a nuisance than their ostensible mission. Instead, this walled-off healthcare system functions like a cost control service for corrections departments, organized around limiting spending and fending off lawsuits rather than actually caring for anyones’ health. In this business, prisons are the customer, not incarcerated people, and a department’s needs take center stage.
While correctional facilities can never be healthcare facilities, there remains an urgent need to improve the healthcare delivered to incarcerated people. Rather than try to medicalize corrections infrastructure, we advocate for an approach that takes as much medical responsibility out of the hands of corrections departments as possible. To conclude this report, we offer a range of recommendations to change who is served by healthcare providers, who’s in control of care, and which outcomes should signal a successful service. These recommendations include shifting the incentives that shape healthcare delivery by removing healthcare from the corrections bureaucracy, moving toward public provision of care, and decarceration and investment in public health infrastructure. We also recommend ways to achieve and defend a higher standard of care for incarcerated people by developing uniform quality performance indicators; greater oversight, accountability, and transparency; and dismantling unnecessary obstacles to litigation for incarcerated people.
What’s driving correctional healthcare policy? It’s not healthcare.
While the broader U.S. healthcare system poses many obstacles to obtaining care in the community, incarcerated people face an even more bizarre and unnecessarily complicated healthcare system that is arguably even more restrictive and dismissive. Correctional healthcare is designed in such a way as to disregard a patient’s needs, experiences, or desired outcomes unlike the patient-centered care model common to this country.
Instead, medical spending3 and deference to the routine operations of correctional facilities4 shape medical providers’ relationships with incarcerated people.5 Healthcare policies sometimes specify that departments only provide healthcare that is “medically necessary” or “essential.”6 As a result, incarcerated people face limitations that other people typically don’t: they can’t choose their doctors or seek second opinions, and they can’t choose to go to a hospital or emergency room — even if they wanted to pay for it themselves. Their needs are frequently downplayed or ignored by staff; their treatments are routinely delayed, altered or ended, contradicting the orders of outside providers; and they are distrusted as “malingerers” who are prone to lying to healthcare providers.
Several incarcerated people told us that standard procedure in their facility was to first bring healthcare concerns to corrections officers, who would then contact medical staff on their behalf. This inability to contact medical directly meant it was common for officers to delay or deny their requests; in other words, officers were effectively making medical decisions themselves. Additionally, several people said officers would remain in the room for medical appointments, their presence discouraging people from speaking freely about their health because officers tended to gossip and leverage their health needs against them.
Corrections officers do play a role in our ability to access and receive medical care, because if we go to the clinic we must first report that to them and ask them to call the clinic. It is customary for them to ask what the problem is, and I know that sometimes women feel that it is a privacy violation to have to explain their issues to corrections officers. For example, if someone has a herpes breakout, or a yeast infection, they might not want to have to report that to an officer, especially if it’s a male officer. I know that I have sometimes heard women asking the officer to call the clinic for them, and I have heard officers refuse to do so just because they might believe that the incarcerated individual is [on] loss of recreation status and just trying to get out of their cell by going to the clinic. However, COs are not medical experts so they shouldn’t be blocking a person’s access to healthcare by refusing to call medical upon request.
— Pamela S.
On a one-to-one basis, the nursing staff seems very polite and professional, even friendly. In five years of incarceration in Nevada, I have never seen a doctor in prison, despite being 64 and having multiple chronic medical issues. I interact with nursing staff at least twice daily when I get checked for blood sugar/insulin. However, nursing is horribly understaffed here. Getting timely refills of common medications is terribly difficult, nearly impossible sometimes. Nothing is automatic and when any prescription expires, there is a circular black hole of bureaucracy trying to get either a renewal or reexamination. Occasionally I come into the infirmary for a review of my charts. Nobody says anything but I believe the nurse practitioners must be visiting because they frequently prescribe medication or outside doctor referrals that are never followed through on. Of course, it is almost impossible to get any minor medications from bandaids to cold and allergy medications. We are rarely told “no” directly. The most common protocol for all inmate support is to merely ignore undesirable requests and deny it later.
Whenever we have to speak to medical or mental health staff about any issue, it is often done in the presence of custody staff. NONE of them appear to be trained in HIPAA privacy issues. As concerning as this is, it is less problematic when we are actually at the infirmary. The officers present don’t normally know us or interact with us. Unfortunately, most medical and mental health consults occur in the housing units, near custody staff that we deal with on a daily basis. These custody staff members are notorious for using personal medical and mental health information for leverage and/or public humiliation. Despite warnings, medical staff seem oblivious or unconcerned.
— Wayne V.
It’s often said that people in prison “have a constitutional right to healthcare.” This is technically true, but it’s sometimes taken as meaning incarcerated people have access to more or better care than everyone else. In practice, this “right to healthcare” simply means that corrections departments can face legal penalties if (and it’s a big ‘if’) a court determines they have inflicted “cruel and unusual punishment” by denying medical care in such a way that amounts to “deliberate indifference to serious medical needs.” Far from a proactive guarantee of healthcare, this highly specific legal test is a defensive tool available only after grave harms occur, and it requires a difficult, lengthy, costly court battle to use it. The lack of a proactive healthcare quality guarantee means that even the most basic, routine medical attention is frequently withheld from incarcerated people.
Incarcerated people’s “right to healthcare” came from a 1976 Supreme Court ruling in the case Estelle v. Gamble, which created the standard that “deliberate indifference to serious medical needs” violates the Constitution’s Eighth Amendment prohibition on “cruel and unusual punishment.”7 Estelle’s “deliberate indifference” standard created a high bar that incarcerated people have to meet to contest medical neglect and mistreatment;8 however, it created a valuable opening in federal courts for incarcerated people to force corrections departments to address their health needs. Between the 1970s and 1990s, incarcerated people used Estelle and other pathways9 in the courts to pursue accountability, better treatment, and more humane conditions. By the 1990s, nearly every state prison system and hundreds of jails were under court-ordered injunctions and consent decrees because of their horrendous conditions of confinement.
Then came the backlash. The Prison Litigation Reform Act (PLRA), passed in 1996, made it much harder for incarcerated people to use federal courts in this way.10 Around the same time, pioneers of privatized correctional healthcare11 seized a market opportunity to help overwhelmed corrections departments deal with the consequences of (1) ballooning prison populations, (2) dramatically escalating healthcare costs, and (3) lawsuits filed by incarcerated people.
Correctional healthcare as a cost control service for prisons
State and local governments are on the hook for funding medical care for people in their custody. However, they’re blocked from receiving crucial federal subsidies to fund that care. While governments can and should invest more in the healthcare of incarcerated people than they do right now, it’s undoubtedly challenging to meet the level of need in prisons without the federal government’s assistance. As a result, their need to control medical spending overrides a concern with providing patient-centered medical care. In other words, one of the biggest reasons why correctional healthcare is so universally bad is that state and local governments have committed to incarcerating people at a scale that they cannot afford to care for on their own.
Correction officers regularly behave as if medical care is a privilege, and it is a privilege that most (all?) inmates do not deserve. It would be easy for inmates to get the impression that custody staff feels that the cost of medical care comes out of their paychecks. This can be easily observed whenever nurses visit the housing units, whether it is to dispense medication, provide insulin, or consult patients. They will say so.
— Wayne V.
I feel medical providers want to save the state money. It seems here, no matter what, one provider always tells us to drink more water (which is polluted because we are on a superfund site) and to lose weight. Like that is the answer to all medical problems. No, I don’t feel like our input or preferences matter because medical staff don’t care that we don’t have access to good food or other items not listed on our canteen or in the chow hall.
— Anonymous at a women’s facility
Money is the deciding factor of prison healthcare. Delay in treatment, especially surgeries, MRI, or other expensive procedures, can most likely be delayed by citing scheduling backlogs, staffing shortages in transportation, or poor communications from the clinic/hospital, to the vendor, to the inmate, on such things as stopping certain medications prior to surgery, fasting, and other such requirements before seeing an outside physician.
— Joe M.
Indeed, correctional healthcare represents a serious financial burden even for large cities and states, but especially for smaller and more cash-strapped jurisdictions. For fiscal year 2015, Pew Charitable Trusts and the Vera Institute of Justice estimated that the typical state Department of Corrections spent $5,720 per incarcerated person to provide healthcare services including medical, dental, mental health, and substance use treatment.12 Overall, they estimated that 49 state corrections departments collectively spent nearly $8.1 billion on healthcare that year.
In the “free world,” Medicaid provides essential federal funding for hospitals, community health centers, physicians, and nursing homes serving over 82 million people — funding that smaller governments could not come up with on their own. However, corrections departments are blocked from receiving these crucial federal healthcare subsidies because of Medicaid’s “Inmate Exclusion Policy,” which prohibits the use of Medicaid funds to “pay for the health care of an ‘inmate of a public institution.’”13
Private correctional healthcare providers see this funding dilemma as key to winning and maintaining lucrative contracts, and design their offerings around keeping costs down above all else. There are two implicit components to these offerings: (1) daily practices that actively limit the care provided to incarcerated people, and (2) reimbursement models where profits hinge on cost cutting and financial restraint rather than care outcomes. Some of the most common day-to-day cost control tactics include:
- Refusing, limiting, or altering treatments and prescriptions14 — including outright denying medications and treatments prescribed by doctors outside of the correctional setting or that people may have received for months or years prior to their incarceration. Multiple incarcerated people told us that, when altering prescriptions, correctional healthcare providers often underprescribe or favor cheaper options15 regardless of their efficacy or side effects.
- Denying and slow-walking care, including delaying exams and medical attention as long as possible. Several incarcerated people noted that “take tylenol,” “drink water,” and “lose weight” are among the most common responses to (often serious) medical needs. Prison medical staff might also deem treatments “elective” and “not serious” in contradiction of outside providers, and avoid sending people to hospitals and outside specialists until the last minute (or request prompt discharge) to reduce hospitalization and transportation costs.16
- Limiting staff expenditures, often understaffing facilities and/or favoring workers with lower-level credentials or spotty records. In some places, this involves staffing Licensed Practical Nurses heavily and having them provide care without the input of Registered Nurses and physicians.17 There are also what’s known as “circuit rider” physicians who provide limited attention to thousands of incarcerated people over a large geographic area.18 Several incarcerated people we heard from said they felt rushed and that they had limited time to speak with medical personnel because of the conduct of a provider or corrections officer.
- Severely limiting and/or rejecting patient preferences, preventing them from influencing the care they receive. This includes a general belief that incarcerated people lie about or exaggerate medical conditions, and a provider culture in which healthcare providers are encouraged to be deeply suspicious of their claims.19 Incarcerated people are generally offered healthcare on a ‘take it or leave it’ basis, and are not offered opportunities to seek second opinions or alternate providers. Blanket suspicion and disinterest in care preferences and goals were common themes in the feedback we heard from incarcerated people around the country.
When it comes to reimbursement models, legal scholars Micaela Gelman and Dan Weiss have explained in detail how correctional healthcare business models directly link their profits to their ability to pass savings on to departments. Three of the most common business models — “fixed-rate,” “cost-plus,” and “aggregate cap” — are described in the table below. Each model has different payers and produces different financial incentives, but they all effectively prioritize contractor profits and corrections budgets over the actual healthcare needs of incarcerated people.
| Business model | Who pays, and how? | What are the financial incentives? |
|---|---|---|
| Fixed-rate20 aka Managed care or Capitation | The government pays the contractor a flat rate21 per incarcerated patient, regardless of the medical needs of people in their care. | Every dollar that does not go to care becomes profit for the contractor and they lose money if spending exceeds cost projections. Governments don’t see any savings if less money is spent, but they also don’t have to pay extra if more is spent. Governments also get a relatively predictable picture of their total spending (absent fluctuations in the prison population). |
| Cost-plus aka Cost-sharing | The government reimburses the contractor for all expenses and pays an additional fee for arranging and managing care.22 | Governments save money when incarcerated people utilize fewer/less expensive services than budgeted, incentivizing contractors to suppress costs in hopes of contract renewal. |
| Aggregate cap | Contractor pays the first several tens of thousands of dollars for high-expense services (e.g., emergency, off-site, specialists). Expenses that exceed this cap are covered by the government. | Contractors are incentivized to reduce services (denying care or attempting to ‘treat’ everything in the infirmary) to minimize expenses and/or reduce cost exposure for governments, which in turn helps to ensure contract renewal. |
Proponents of privatized correctional healthcare argue that free market competition weeds out bad actors and punishes those who deliver poor care, rewarding firms that provide the best quality and most economically efficient delivery of healthcare. While this sounds nice, in practice it’s been demonstrably false: as we have seen in countless correctional facilities across the country, providers have no problem landing new contracts and renewals despite horrific care, bad press, mounting annual healthcare costs, and lawsuits. Contrary to the free market’s promise, many of the worst providers survive, sometimes thanks to bankruptcy laws that rescue them from the consequences of their actions and leave incarcerated people in the dust (which we describe in detail in the next section).
Indemnification: Shielding corrections departments from lawsuits
The overwhelming focus on costs means that incarcerated people are routinely denied adequate healthcare, and corrections officials and medical providers are inevitably sued as a result. For this reason, correctional healthcare providers take extra care in shielding department officials from these costs, relying on what’s known as “indemnification.” While it’s common for contracts to include indemnification provisions, in this setting these provisions are often used to avoid accountability for medical abuse and neglect.
Although these doctors or specialists give certain orders for the prison to go by they still ignore these orders and disregard prisoners’ healthcare needs. Whether it’s a chronic illness or disease or for treatment for vital organs, prison officials don’t take our healthcare seriously and are anticipating civil suits because they believe they will win, and because prisoners have to prove so much against prison officials. The care that I get off site is comforting because I feel a sense of compassion from medical staff who are not a part of prison med staff.
— Roderick H.
Indemnification is a legal term that means to “hold harmless,” and it’s an important part of provider contracts. If an incarcerated person sues over medical care, these contracts specify that that the contractor will assume some or all of the financial risk of the lawsuit.23 Indemnification can take different forms: a “joinder,” for example, allows government officials to attach their contractor and its personnel to any lawsuit they face over healthcare. Some contracts require providers to reimburse or pay outright the government’s legal defense costs, or renounce the government’s responsibility to cover the contractor’s portion of those costs. Private providers also purchase insurance policies that can help cover litigation expenses. These various provisions exist because the Supreme Court has ruled that state and local governments outsourcing essential services to private companies are still liable for their conduct. As scholar Dan Weiss notes in his examination of privatized correctional healthcare, indemnification defangs these rulings and makes them “symbolic.” Ultimately, when contractors insulate government officials from the consequences of bad healthcare, they remove strong incentives for governments to do better.
Contractors also shield governments by making it harder for the public to see what’s going on. Private contractors are not subject to the same public disclosure requirements as government agencies, which can make it harder to obtain information about their work that would otherwise be disclosed.24 Some providers go a step further, reserving a right in their contracts to refuse to disclose settlement information to governments (i.e., to their own clients). This gives governments some plausible deniability, limiting their ability to audit providers’ involvement in lawsuits, insurance payouts, and case outcomes. In other words, it’s harder to hold a government accountable for working with an infamously bad provider if that government doesn’t have evidence of the provider’s track record.
Downstream of these business decisions, contractors have had to find ways to keep their businesses alive after assuming so much legal and financial risk. One popular strategy is to look to Texas, where a legal defense known as the “Texas 2-step” allows companies to file for bankruptcy, split into two parts, and load one business with the assets and the other with debt. Freed of its debt and legal liabilities, the rebranded company is then free to pursue new contracts again. This maneuver significantly complicates incarcerated people’s ability to obtain settlements from these companies. Corizon — one of the most infamous correctional healthcare providers — declared bankruptcy in 2023 and split into Tehum Care Services (which took on all the debt) and YesCare (which took on all the contracts). YesCare still exists today, with hundreds of millions of dollars in contracts inherited from Corizon. Sometimes this practice is so blatant that the new entity has the same exact address as the one declaring bankruptcy.
Public care might be better than private, but it’s no cure-all
Privatized correctional healthcare is bad, but publicly-provided care will not necessarily fix everything. As government actors, public providers like public universities and health agencies could be more transparent and more responsive to public pressure. Unfortunately, public providers face some of the same constraints as private ones: both are at the mercy of limited budgets and operate within the corrections hierarchy, where healthcare decisions take a backseat to security and the orderly operations of corrections facilities.25 Additionally, public employees are not necessarily more compassionate toward a highly stigmatized and politically disempowered patient population, and they may still engage in discrimination against people based on race, gender, disability, and other factors, as happens elsewhere in the “free world” healthcare system. While ending for-profit healthcare provision is useful, it’s even more important to break down the wall between healthcare in prison and healthcare in the community. In other words, publicly-provided care is not enough unless it is significantly less constrained by the prison bureaucracy and its prioritization of officer discretion and orderly operations.
In prison you can feel — even if it’s not said aloud — that you are a dollar sign, the path of least resistance to get the most available means of profit. Often brushed aside, denied, [and] commonly delayed. On the outside, we have more options; when the medical providers know that they are the only option they seem to become arrogant and feel that they are without reproach. When I was on the outside I could receive immediate medical attention whenever I needed it. Here you must wait until you are called unless it’s an extreme emergency.
— Emanuel W.
I feel like I could access good care outside of prison, even if it was a free clinic. Here in prison they always act like we are faking an illness or taking money away from DOC. We have offered to pay for our own services or inmates want to buy/upgrade their medical by buying their own health insurance. Colorado DOC won’t let us but complain we are “faking it.” I never experienced that in the “free world” or to be told to just “drink more water” or ” lose weight.”
— Anonymous at a women’s facility
I was equally poor before prison and on state healthcare prior to incarceration and I recall a number of hoops to jump through out there as well, however eventually I got care out there, physically anyway. In here that is not the case. The hoops in prison are not only for us but also for medical staff, and the ridiculousness it takes to get anything done is exhausting and designed to make people give up.
— Shajiyah I.
There really isn’t much data to back up the assumption that public providers are actually better than private ones, in large part because correctional healthcare data and standards vary so widely that it’s difficult to compare them. However, there have been some attempts to compare public and private providers, specifically in jails. In 2020, Reuters published an in-depth review of healthcare in over 500 jails, looking at deaths from illness and medical conditions, suicide, and acute effects of drugs and alcohol. They found that, between 2016 and 2018, “those relying on one of the five leading jail healthcare contractors had higher death rates than facilities where medical services are run by government agencies.” According to Reuters, jails with public medical providers (usually provided directly through a sheriff’s department or local health agency) averaged 12.8 deaths per 10,000 incarcerated people. Meanwhile, death rates among the top five private providers ranged from 15.1 to 20.2 annual deaths per 10,000 incarcerated people. In other words, private providers had between 18% and 58% higher mortality rates (depending on the provider) in jails compared to those with public providers.
Another analysis of this same dataset by scholar Michael James Zoorob produced conflicting results: Zoorob found that privatization did not increase mortality, including when analyzed over four years of a private medical contractor providing care. However, the results did vary between states: some saw a rise in deaths with privatization while others did not. Zoorob suggests there “may be important roles played by monitoring and other elements of local contracts” that can help explain these variations. Additionally, privatization was associated with significantly increased medical spending, rather than the savings these providers promise. Zoorob writes that these results could also potentially be explained by public providers not being more attentive, altruistic, or amenable to public pressure or accountability, as many assume.
These conflicting results complicate the argument that ending privatization is enough to meaningfully respond to this healthcare crisis, and underscore the urgent need for more data collection and analysis with regard to healthcare outcomes in jails and prisons. But they also suggest a broader issue: that positioning healthcare delivery within corrections departments, where the mission to punish people overtakes any interest in caring for them, is a major obstacle that needs to be confronted.
Getting away with murder: Correctional healthcare “accountability”
How have corrections departments and their medical providers gotten away with so much harm for so long? Some answers are familiar for incarcerated people and their advocates: corrections oversight in the U.S. is in relatively early stages of development, especially when it comes to healthcare. The U.S. has been making encouraging progress on this front but still lags far behind its peer nations.26 In this section, we review the various forms of correctional oversight, quality control, and accountability to spotlight what exists and where gaps remain.
The complicated world of corrections oversight
The courts provide the primary venue for oversight and accountability in jails and prisons, but as we’ve explained, this provides very limited protection for incarcerated people. In addition to the courts, incarcerated people could benefit immensely from robust, independent, and external oversight that ensures higher standards for both living and healthcare conditions.
Most states have some form of oversight regarding healthcare, whether it’s oversight bodies focused exclusively on healthcare or oversight bodies whose broader focus overlaps with healthcare. Scholar Michele Deitch has argued that independent, external oversight tends to be far more cost effective than court oversight. It’s also better at exerting informal pressure on staff and agency behavior because they know they’re being watched. However, correctional healthcare oversight varies significantly in its focus and implementation between jurisdictions, and it’s often a responsibility left to corrections departments to carry out. In many cases, this oversight is focused on ensuring certain processes are in place rather than certain healthcare outcomes are being achieved.
Healthcare oversight. To make sense of the correctional healthcare landscape, we turned to two studies for help: a 2011 RAND Corporation study, and a 2017 survey of healthcare quality, standards, and oversight from Pew Charitable Trusts. The RAND study analyzed data from Missouri, New York, Ohio, Texas, Washington, and the federal Bureau of Prisons, and found that each system was doing something to monitor quality, but the number, types, and origins of their quality measures varied substantially. Most importantly, while many of the standards had process measures associated with them (for example, how quickly services were delivered) they were not designed to assess whether evidence-based recommended care was provided and whether desired outcomes were achieved.
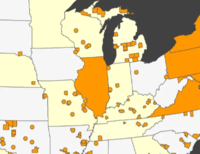
The 2017 Pew survey also found that there are no uniform quality of care standards for corrections, and no mechanisms for reporting comparable performance data between states. While this survey is now almost a decade old, it remains the most recent accounting of the healthcare oversight landscape available. Pew found that nearly every state assigns monitoring27 responsibility to the departments of corrections themselves 28 — a troubling conflict of interest given the cost-cutting and lawsuit-avoiding incentives described earlier in this report. Seven states 29 share responsibility for monitoring with their health departments. Only South Dakota has a wholly independent monitoring system operated by its departments of health and social services.30 Twelve states did not meet Pew’s criteria for a healthcare quality monitoring system,31 and three states did not respond to Pew’s survey at all.32
Even aspirationally, quality and performance measures should not necessarily mirror community care standards. This is because there are significant differences in disease prevalence, premature aging, short periods of incarceration, and limited functionality/linkage between community and prison clinical systems. Instead, the emphasis should be on achieving equivalent outcomes rather than equivalent care delivery. In other words, the needs facing populations inside and outside of prisons are different enough that “adequate care” should be judged on the basis of achieving similar healthcare outcomes rather than receiving similar care.
There are many newer healthcare oversight models being developed, according to a 2022 scoping review published in the journal Health Justice. But one crucial drawback among all of those featured in the review is that none of them included patients’ perspectives. This represents a significant gap in the scholarship; patient experience is a core component of evaluating community care and the same should be true for incarcerated populations.
Corrections oversight. In addition to healthcare-specific oversight, it’s worth considering the larger universe of corrections oversight because of how it overlaps with conditions that impact peoples’ health. In scholar Michele Deitch’s 2020 survey of corrections oversight, But Who Oversees the Overseers?, she found most local jails have minimum standards that are overseen at the state level.33 In these states, sheriffs are often involved in writing the standards, and they tend to be minimal and vague34 since they have to apply to facilities ranging from large urban to small rural jails. While there are inspections to determine compliance with those standards,35 the consequences for failing to meet standards are often limited,36 and agencies frequently receive waivers or variances that allow them to continue their work while out of compliance. Local oversight of jails is far more rare, but exists in many forms across a smaller group of states and individual counties. These local bodies have some advantages: they create opportunities for the local involvement of citizens in the oversight process and, since county governments are often responsible for funding local jails and shouldering some legal liability for their conduct, local leaders can more effectively insist on transparency around conditions.
Meanwhile, in prisons, Deitch found that in most cases oversight is designed so one state agency oversees another. However, oversight agencies vary greatly in terms of design, purpose, size, staffing, scope of authority, and access to facilities.37 In the end, existing oversight systems are inconsistent and generally lack the enforcement power and resources needed to ensure correctional healthcare is up to standards — however low those standards may be.
Accreditation
Many corrections departments are accredited by the American Correctional Association, while medical staff can receive accreditation from the National Commission on Correctional Healthcare. Given the lack of uniform standards, quality measurements, and robust oversight, accreditation is generally viewed as a positive effort toward ensuring good healthcare outcomes. In fact, even facilities that are not accredited still use the standards of major accreditation organizations as guidelines for how to structure their services.
While accreditation can be useful in some cases, it’s not a substitute for actual standards or oversight. Accreditation agencies are not objective observers, having played important roles in the expansion and public perception management of mass incarceration. On the plus side, accreditation is geared toward ensuring compliance with specific standards, with a focus primarily on management matters and benchmarking specific operations and procedures. According to scholar David Bogard, accreditation organizations like the American Correctional Association have increasingly moved towards outcomes-based standards rather than exclusively process-based standards since roughly 2001. The organization’s “mandatory standards” for accreditation include many aspects related to critical healthcare concerns, but the standards overall constitute a bare minimum required to comply with constitutional requirements (which, as we’ve already noted, sets a very low bar). In simpler terms, while some research points to accreditation’s benefits for health and post-release outcomes, many facilities with abhorrent conditions are nonetheless accredited. As scholars Spencer Headworth and Callie Zaborenko have argued, accreditation can function as a defensive, reactive measure rather than a proactive, proscriptive one.38 According to their analysis, corrections departments pursue these endorsements to bolster their reputations in a stigmatized and litigious field, which can work to temper and deter actual legal challenges.
Litigation
Lawsuits are the main way incarcerated people can pursue accountability when their healthcare needs are not met. Incarcerated people have various legal pathways to challenge inadequate care, some of which depend on whether they’re incarcerated at the state or federal level. However, there are significant drawbacks and limitations associated with having litigation as the primary form of oversight and accountability.
Incarcerated people can sue for injunctive relief to stop certain actions or demand departments take others, or to secure monetary damages to compensate for the harm they endured. Both constitutional claims and federal legal claims (like those brought under the Americans with Disabilities Act) require that the incarcerated person show the provider was aware they were being negligent or discriminatory — it’s not enough to argue they simply failed to provide treatment. In addition to federal civil rights lawsuits, incarcerated people can sue for medical malpractice and negligence in state courts. Lawsuits can pressure departments to engage in professionalization and standardization practices, sometimes leading to important improvements in healthcare delivery. Courts also have the power to actually enforce changes in ways that oversight agencies often can’t39 through their ability to institute “special masters” and monitoring teams, or place departments in receivership. As noted in the very beginning of this report, litigation also provides rare (albeit conservative) data points that we can use to gauge the quality of correctional healthcare.
But there are significant barriers to receiving relief through the courts, too. Federal courts are generally concerned with correctional healthcare when it violates federal laws or the Constitution,40 but they aren’t in the business of ensuring healthcare meets a community standard of care or actually delivers desirable outcomes; many facilities with objectively terrible conditions don’t necessarily violate the Constitution. Judges also tend to defer to the decision making of government agencies and avoid engaging in “micromanagement.” Beyond these issues, it’s important to note that litigation is fundamentally limited and reactive, which makes it less useful for enforcing an ongoing standard of care. Lawsuits are focused on very specific people, cases, and factors, and their influence is generally time-limited: once court oversight ends, the funding to continue any oversight or accountability measures the courts put in place disappears, and facilities are at risk of backsliding to their old bad practices.
People incarcerated in federal prisons are at a particular disadvantage when it comes to litigation compared to their peers in state prisons. In particular:
- Unlike people in state prisons, people in federal prisons can’t bring civil rights claims against contractors because they are in federal facilities and are not operating “under the color of state or local law.” So while people in state and local custody can bring federal lawsuits under what’s known as Section 1983 alleging violations of civil rights, people in federal prisons cannot do the same against federal contractors.
- People incarcerated in federal prisons can sue using the Federal Tort Claims Act (FTCA), however this can only be for acts or omissions that result in harm or injury (also known as torts) — not for civil rights violations. The FTCA also has an exemption for independent contractors who are not under the daily supervision of federal employees, meaning that medical contractors are generally exempt from being sued under this law.
- To bring a civil rights action, people in federal prison can use what’s known as a Bivens claim, but these, too, are very limited and difficult to win: Bivens claims can only be brought against individuals, and those claims have to have a “familiar Bivens context,” meaning it has to be the same or similar to what other courts have allowed in previous Bivens cases.
Overall, litigation is an important tool for holding corrections departments accountable for inadequate healthcare. However, it’s so complicated, slow, and fraught that it should not be the only real tool incarcerated people have to push for better care. Instead, additional, proactive measures that ensure a higher standard of care are needed, beyond purely reactive measures that are extremely difficult to employ.
Recommendations: Prioritizing the health needs of incarcerated people over the budget and security needs of prisons
Throughout this report, we’ve examined the structural problems with correctional healthcare and the shortcomings of oversight and accountability measures available to support incarcerated people in securing better healthcare. While these problems are severe and deep-rooted, there are actions that jurisdictions can take to radically shift the incentives and deliver better outcomes. Notably, the U.S. can do this in a way that reduces investments in mass incarceration while building up public health infrastructure.
Our recommendations may preempt one another depending on the politics and situation in a particular jurisdiction (for example, there’s no need to demand greater transparency and accountability from private contractors if a jurisdiction successfully ends privatization). These policy ideas are not a one-size-fits-all slate of solutions but each could begin to shift healthcare delivery incentives and quality.
Shift the incentives that shape correctional healthcare
Decarceration & public health investment. At the most basic level, every person diverted or released from incarceration is someone whose health will not suffer as a result of the neglect and patently unhealthy environments of prisons. This involves the aggressive use of all available release mechanisms, including compassionate release, pre-arrest diversion, parole, etc. Importantly, a decarceration process concerned with healthcare must be linked with significantly improved public health infrastructure. This is a heavy lift, but perhaps the most efficient among our recommendations.
Remove healthcare from the correctional hierarchy entirely. In U.S. prisons, healthcare services reside within corrections departments. They are funded by corrections departments, and are confined by the priorities and operations of corrections facilities as dictated by leadership. Improving healthcare requires breaking health services out of these confines entirely, so that, for example, correctional officers are less able to interfere with requests for healthcare and have less exposure to sensitive health information. Additionally, breaking down the wall between correctional healthcare and community healthcare is likely to both improve quality and ensure better continuity of care when people are released. Continuing medications and treatments from the outside (and not denying recommendations from outside providers), allowing incarcerated people to get second opinions, and insulating medical providers from the punishment imperatives of prison could change incentives that often lead to delayed and denied care.
There have been efforts in the past to remove healthcare from corrections departments, but they failed precisely because they were unable to wrest daily control of healthcare decisions from prison administrations. In other countries, corrections agencies are far more constrained in their ability to deny or delay care for incarcerated people. Norway, for example, delegates oversight and care delivery to community providers. This has many benefits:
- It allows for a structure for community-based providers to deliver care outside of corrections departments;
- It helps resolve staffing quality and quantity issues;
- It resolves ethical dilemmas by separating care from punishment infrastructure;
- It expands what constitutes “care” to nutrition, STI, drug use, perinatal care, etc;
- It leads to better fidelity to community standards by incorporating incarcerated people into public health rather than separating them from it.
Decoupling healthcare for incarcerated people from corrections agencies necessarily involves repealing policies that prevent the federal government from subsidizing incarcerated people’s healthcare. Medicaid’s Section 1115 waivers have been an important step forward, allowing people to receive Medicaid in anticipation of their release, but this does not go far enough — Medicaid’s “Inmate Exclusion Policy” should be abolished altogether to remove the responsibility to pay for care from corrections agencies. Eliminating the exclusion would also open up the Medicaid grievance process for incarcerated people, creating another avenue for care accountability. The good news? Pew’s survey estimates that healthcare accounts for roughly 20% of corrections spending, so federal subsidies could significantly reduce the amount of state and local budgets going to incarceration.
End contracts with for-profit healthcare providers. As we’ve argued in this piece, public providers are likely better than private ones. However, ending privatization won’t solve every problem related to correctional healthcare, and is unlikely to automatically translate to higher quality and quantity of care on its own. Still, it’s worth doing especially if it goes hand-in-hand with removing healthcare responsibilities from correctional agencies entirely. Public care can look like handing medical care over to universities, including creating rotational programs for students, or creating partnerships with public health agencies. In addition to public oversight and influence over healthcare policy, the benefits of public providers include:
- More opportunities for community-oriented services;
- Improved continuity of care in community;
- Reduced costs related to emergency and off-site care as well as litigation;41
- Development of specialized medical services via residencies.
At the very least, states that continue to outsource care should require bidders to detail and report costs for providing certain services during the procurement process, and implement more robust and mandatory healthcare outcome measurements to help fill the data gap.
Achieve and defend a higher standard of care for incarcerated people
Quality and performance indicators for healthcare. It is shocking how little we know about the quality of care delivery inside, and there’s an extreme need for agreed-upon quality indicators and performance measures. One idea is implementing something approximating how the federal government evaluates hospitals (including both carrots and sticks), which could be useful to adapt for measuring care delivery quality. Corrections departments should not be in charge of healthcare delivery, but if that is to remain the case, they should be held to the same standards as the rest of medical infrastructure. This is not because facilities should be reformed into medical institutions, but because they should not be allowed to operate in a grey area that harms incarcerated people. Corrections facilities should be subject to the same state health agency regulation and independent healthcare-specific accreditation as all other major public health infrastructure.
Independent oversight and accountability. Independent, routine, enforceable governmental oversight is essential to ensuring a proactive and ongoing standard of care. In the U.K., for example, the Inspectorate falls under Britain’s Home Office, but remains entirely independent of the prison system. Having independent oversight and accountability would mean:
- Investigations of individual grievances fall to the prison ombudsman, a separate body;
- The oversight is active for all institutions at all times, dictating and maintaining a set of standards and outcomes, not just for the bad ones when a bad thing happens;
- Staff will know they are being watched and could face consequences; and it’s much cheaper than long-term judicial monitoring.
According to scholar Michele Deitch, state-level oversight of prisons is best because the size and variation of state corrections departments varies significantly, making national-level oversight impractical. Local oversight, on the other hand, may work best for jails given both local jurisdictions’ responsibilities for funding jails and the ability to involve people in the area in oversight. Many of these agencies and organizations are relatively new and still coming online, and advocates should work to strengthen them. While some agencies may have their issues, they generally represent a step forward, away from the largely court-centric oversight system that exists today.
Remove litigation obstacles. Litigation is an important tool that should be preserved for incarcerated people. It shouldn’t be the only or primary tool for accountability, but it can be improved immensely in ways that ensure fairness and keep corrections abuses in check. Lawmakers at the federal and state levels can take steps to repair and strengthen correctional healthcare litigation such as:
- Subsidizing medical expert testimony for litigation (as advocated by Medical Justice Alliance);
- Rescinding the Prison Litigation Reform Act to remove onerous obstacles to litigation;
- Legislating a floor for healthcare quality that is more explicit and robust in its demands, and that sits well above the “deliberate indifference to serious medical needs” as defined in Estelle.
- For people in federal prisons, ending or amending the independent contractor exemption to the Federal Torts Claims Act so that the federal government could be held liable for the actions of prison contractors.
Get our latest data & analysis in your inbox!
Appendix: A brief history of correctional healthcare and privatization
The history and development of the correctional healthcare system is crucial to understanding why the system seems so structurally opposed to actually delivering healthcare. Unfortunately, this is not a history that has been recounted in many places. Here, we pieced together a rough timeline and history from a variety of sources. This timeline is likely incomplete, many of its data points are not comparable with one another, and it overgeneralizes developments in different parts of the country, yet we still think these broad strokes are useful to understanding the correctional healthcare landscape today.
Correctional healthcare leading up to privatization
Late 19th-early 20th centuries (1880s-1930s). Under the ‘reformatory’ ideology, prisons had a ‘therapeutic’ mission that included basic medical care, an attribute that was heavily in tension with its other mission: to punish people.42 Some prisons had their own physicians and infirmaries but struggled with limited budgets. During this time, some incarcerated people were subject to medical experimentation and other abuse and mistreatment.
Mid 20th century (1930s-1970s). While prison healthcare was never great compared to the community, it appears to have nonetheless deteriorated as the ‘reformatory’ ideology of the earlier half of the century gave way to the ‘tough on crime’ movement coalescing in the 1970s. Under these conditions, prison healthcare was frequently described as limited and barbaric. Poor medical care, sometimes provided by untrained and un/under-licensed medical corpsmen or other incarcerated people acting as ‘nurses,’ helped spark prison rebellions leading into the 1970s, which influenced reform movements.
During this period, local jails (which often provided no healthcare at all) began switching to a ‘direct service model,’ in which they hired their own physicians, similar to what existed in state and federal prisons. But uptake appears to have been slow. A 1972 survey of 1,159 jails found:
- 65% offered only first aid;
- 17% offered no internal medical services;
- Over 30% had no regularly available physicians;
- 80% used unlicensed nonmedical staff, including other jailed people.
Late 20th century (1970s-1990s). Prisons and jails increasingly contracted out healthcare services to other government agencies (i.e., public health departments), hospitals, and nonprofits. Inadequacies continued but seem to have improved to some degree. Issues persisted with staffing doctors who had records full of misconduct or worked with restricted licenses43 that prevented them from practicing in the community. Exploding costs, a growing and aging population, and a turn against government spending in the Reagan years encouraged a turn to privatization.
Privatization takes over correctional healthcare
People who supported privatizing correctional healthcare argued that doing so would:
- Save governments money;
- Allow for more efficient health service delivery;
- Produce quality care outcomes via the ‘invisible hand’ of the market;
- Reduce government bloat and vulnerability to pesky ‘special interest groups.’
1999: A survey of 27 state prison systems found 32% had privatized healthcare.
Costs explode (2001-2008): 42 states saw a substantial rise in total correctional healthcare spending, with a median growth of 49% during this period. In 35 states, per-person spending on healthcare had a median growth of 28%.44
2004: 32 states contracted “some or all” prison health services.
2007: 40% of total correctional healthcare spending went to the private sector.
2007-2009: In New York state, 70% of local jails contracted with local providers, 14% with private corporations, and 16% with public facilities—but privatization disproportionately affected people of color in urban jail populations.45
2013: 30 states had privatized prison healthcare delivery.
2016: More than half of all state prisons and local jails privatized care, and the private correctional healthcare industry was valued at $3 billion. According to a survey by Pew Charitable Trusts in 2016,46 most state prison healthcare systems relied upon a mix of outsourced and state-employed clinicians:
- In 17 states, the majority of healthcare services were directly managed and provided by the state.47
- Twenty states contracted out most healthcare service delivery.
- Eight hybrid states provided healthcare via a roughly-even mix of state and contracted employees. 48
- Four states worked with a state medical school or affiliated organization.49
2016-2018: 60% of large local jails (with an average daily population of at least 750 people) had privatized medical care.
2018-2019: Over 90% of the 34 southeastern U.S. jails surveyed responded that they contracted with 12 distinct private companies.
2019: Around 70% of jails with staff accredited by the National Commission on Correctional Healthcare reported outsourcing care.
2022: The correctional healthcare industry was estimated to be worth $9.3 billion — a 213% increase in six years.
Footnotes
This is a significant underestimate of the litigation landscape related to correctional healthcare. Here, we are only talking about court orders directing departments to take or not take particular actions with regard to prison healthcare — we are not counting cases that only resulted in monetary damages, of which there are many, many more. Additionally, this count also does not include court actions taken against local jails, of which there are thousands in the U.S. ↩
Quotes from incarcerated people featured in this report were obtained with their permission and guidance on attribution. Out of an abundance of caution due to the risk of retaliation, we are withholding the state, name of the facility in which they’re being held, and their last names. ↩
Major components of correctional healthcare spending include the cost of staff, supplies, medications, treatments, or procedures, as well as corrections staff time for transportation offsite. ↩
Healthcare delivery is shaped by deference to prison operations in many ways, including the timing of sick call or onsite medical staff hours, or whether an officer wants to contact the infirmary or escort someone to it. Notably, much of this comes down to the discretion of corrections staff. ↩
To be clear, this is not a matter of the individual conduct of medical staff, but rather how the structure of healthcare delivery in prisons leads to poor outcomes. While many incarcerated people did not have great experiences with healthcare workers in prisons, many did and said they knew they were doing the best they could in a tough situation. ↩
The Bureau of Prisons’ healthcare policy (Health Services Administration Policy No. 6010.05) specifies that incarcerated people will receive “medically necessary” healthcare, that it “must be delivered within the constraints of correctional concerns and responsibilities,” and that “medical services provided to Federal inmates will be obtained at the lowest possible cost.” ↩
For a thumbnail history of the rise of privatization in correctional healthcare, see Appendix. ↩
In addition to legal challenges, incarcerated people contested their poor medical care in a variety of other ways, including through organizing and rebellion. For example, the second demand during the 1971 rebellion at Attica was for “a change in medical staff and medical policy and procedure. The Attica Prison hospital is totally inadequate, understaffed, and prejudiced in the treatment of inmates. There are numerous “mistakes” made many times; improper and erroneous medication is given by untrained personnel. We also demand periodical check-ups on all prisoners and sufficient licensed practitioners 24 hours a day instead of inmates’ help that is used now.” Two other demands relating to sanitary conditions and food quality also relate to the health of incarcerated people. ↩
A 1977 decision in the case Ingraham v. Wright also established a Fourteenth Amendment claim for inadequate care as well, setting a similarly high bar where an incarcerated person must show a provider’s reckless disregard for their health. ↩
Under the PLRA, incarcerated people have to exhaust all administrative remedies before filing suit, or risk having their suit thrown out. In practice, this means engaging in complicated, time-consuming grievance procedures and seeing appeals through to the end before being able to initiate a complicated and time-consuming process in the courts. Once it gets to court, incarcerated people must pay all court filing fees in full, which is exceedingly difficult given how little money most people in prison have. Dismissals for lawsuits deemed “frivolous” result in strikes, three of which prohibits people from suing again unless they pay their entire filing fee up-front. The law not only delays lawsuits, but it also discourages a lot of people from filing them in the first place. While PLRA applies to the federal courts, many states have similar laws that apply to state courts. ↩
For detailed examinations of the rise (and deregulation) of managed care organizations and their influence on prison healthcare, see scholar Holger Sonntag’s 2017 law review article, Medicine Behind Bars: Regulating and Litigating Prison Healthcare Under State Law Forty Years After Estelle v. Gamble and Richard Seiver’s 2019 law review article, HMOs Behind Bars: Constitutional Implications of Managed Health Care in the Prison System. ↩
In terms of the range of healthcare spending in prisons, California, New Mexico, Vermont, and Wyoming spent over $10,000 per incarcerated person, while Alabama, Indiana, Louisiana, Nevada, and South Carolina spent less than $3,500 per incarcerated person. ↩
The linked Congressional Research Service brief points out some notable nuances and exceptions to this rule. Medicaid funds can be used to cover healthcare expenses when an incarcerated person is a patient in a medical institution that is “organized for the primary purpose of providing medical care” (i.e., a hospital). Medicaid can offset a portion of the costs for in-patient treatment of incarcerated people that extends beyond 24 hours in a qualifying medical institution. Additionally, because of how the Centers for Medicare and Medicaid Services defines “inmate,” people on parole or probation, under home confinement, living in halfway houses operated by state or local governments, or others who otherwise have “freedom of movement” can receive federally subsidized healthcare coverage. Finally, it’s worth pointing out that since outpatient care or care that happens within prisons is considered to take place in a correctional (and not medical) setting, these correctional facilities can, among other things, limit personal privacy, restrict choice of physician, and use nonmedical restraint — all of which would disqualify facilities from obtaining certification as a Medicaid provider. ↩
Maine’s former Corrections Commissioner Joseph Ponte went on a crusade to cut prescription medicines for incarcerated people during his tenure. As the Bangor Daily News reported in 2012: “Since he took the post, Commissioner Ponte has pledged to reduce costs within his department and has said recently that progress has been made. For instance, under the previous administration, there were seven prescriptions on average per inmate, he said. That already has been reduced to an average of five.” ↩
A 2016 survey by Pew Charitable Trusts and the Vera Institute for Justice notes that departments struggle to afford medications for incarcerated patients; they buy “many of the same drugs as do Medicaid agencies […] yet [Departments of Corrections] are not eligible for the federal Medicaid Drug Rebate Program, which requires drug manufacturers to enter into a rebate agreement in return for Medicaid coverage of their products.” The survey goes on to note that states that outsource healthcare to private providers who also are responsible for drug purchasing must “put monitoring in place to guard against the built-in incentive for a contractor to delay prescribing, underprescribe, or prescribe a less expensive but less effective or less well-tolerated medication. This might occur because the cost of the prescribed drug would come directly out of the per inmate fee the vendor receives from the state.” In some cases, a separate provider is tasked with drug purchasing, in which case the opposite incentives for abuse must be monitored: “This might include overprescribing brand-name drugs or overrelying on drugs in a situation where “watchful waiting”—to see if symptoms resolve on their own—or a nonpharmaceutical treatment such as physical therapy, psychotherapy, or even surgery (treatments that the contractor would be obligated to pay for in contrast to pharmaceuticals that these states carve out) might be more appropriate.” ↩
While this report is focused on prisons, it’s worth noting that a common practice in local jails is to neglect health needs until they reach crisis levels, and then temporarily release people from custody to avoid having to pay their hospital bills. ↩
For a quick breakdown of the key differences between Licensed Practical Nurses (LPN) and Registered Nurses (RN), see this explainer from Regis University. Essentially, LPNs receive less training and certification than RNs. ↩
As this report’s author covered in a 2015 investigation into private jail medical provider Advanced Correctional Healthcare, “[Circuit riders] serve as the site physicians for more than one jail at a time, managing the healthcare of hundreds of [detained people]. These doctors are also on-call to fill in for one another in the event they can’t make their shifts. Although [some contracts] stipulate their site physicians are supposed to visit their jails once a week, the majority of their day-to-day care is provided over the telephone because the doctors usually live far from the facilities to which they are assigned. Under this arrangement, [complaints from incarcerated people] are often first evaluated by the jail’s staff. If a nurse or medical assistant can’t manage the complaint on their own, they call the site physician.” ↩
The Chicago Reader reviewed a 2008 staff manual for the correctional healthcare provider Wexford, which includes details that align closely with many of the findings in this report. The manual (the authenticity of which Wexford refused to confirm or deny) urged providers to be skeptical of their incarcerated patients as a default orientation towards them. According to the Chicago Reader’s report, the manual recommended that providers “not to tell patients when their next appointment is, inform patients about their specific diagnosis, give patients any documentation about their treatment plan, offer patients any ‘equipment or supportive aid,’ or attend to any medical problems besides the one they’d been sent for.” It told providers: “DO NOT EVER explain symptoms you would expect to see to confirm a diagnosis to an inmate. If you should, those symptoms will likely be present with the next visit.” Additionally, the Wexford manual claimed that “physical therapy is ‘often abused’ by incarcerated patients, and they warn doctors to be cautious when giving a patient a prosthetic limb.” The Chicago Reader quotes the manual as saying “our patients are often very skilled, and can make serious weapons from innocuous materials.” ↩
As of fiscal year 2015, 19 out of 27 states that contracted out correctional healthcare used the “fixed-rate” reimbursement model, making it the most common, according to a survey by Pew Charitable Trusts. ↩
It’s important to note that fixed-rate reimbursement arrangements produce less useful data. Because governments are paying a fixed-rate to cover a basket of healthcare services, the underlying spending data on particular goods and services are often not made available to governments or the public unless explicitly required in the contract. ↩
Compared to the other models, cost-plus reimbursement models encourage relatively more transparency simply due to the reporting requirements for reimbursement. ↩
In case there was any doubt that contractors see indemnification policies as core to their marketing to governments, take it from Todd Murphy, a director of business development for California’s largest private provider of healthcare to jails and prisons, Correctional Medical Group Companies. In 2016, Murphy told The Guardian that “the main reason counties are choosing to outsource their jail healthcare is not to reduce daily costs, but for the comfort of knowing that a lawsuit brought by the family of a dead inmate would be brought against the company and not the county. ‘We provide a full partnership to our county partners,’ he said. ‘But the biggest thing we do is indemnify the county against risk and [liability], do everything we can to keep them out of trouble.’” ↩
The Human Rights Defense Center (HRDC) has argued that this is not exactly true: the organization has “repeatedly and successfully sued private healthcare companies under state public records laws to bring them under the scope of such laws.” Instead, the obstacle to transparency may be more that litigants either wrongly assume that information is shielded from public release, or have not tried to pursue it the same way HRDC has. ↩
The Wexford manual obtained by the Chicago Reader explains “healthcare roles” in the prison setting, noting that the warden sits at the top of the hierarchy. Wexford’s manual notes that wardens are “responsible for everything that happens in the unit. Although on occasion a medical decision may be in conflict with [the warden’s] express wishes, most decisions should respect [the warden’s] management responsibility.” Additionally, Wexford writes that, “Security is the prime objective of all prison operations, and you are expected to understand and respect that responsibility.” ↩
For more information, prisonoversight.org has built a useful 50 state tracker that helps the public learn about and understand the prison oversight landscape. ↩
Monitoring took different forms in different jurisdictions, but Pew defined it as having four key characteristics: (1) Grounded in data; (2) Established and overseen by state agencies; (3) Applied broadly and consistently across facilities; and (4) Operated on an ongoing basis. ↩
Kentucky is an outlier in that it does not apply oversight to every facility in the state. ↩
Arkansas, California, Indiana, Massachusetts, Nevada, New York, and Washington share responsibility with their health departments. California also shares responsibility with its Inspector General. ↩
In South Dakota, healthcare quality is monitored by the state’s Department of Health, which provides medical, dental, and optometry services in state prisons. The Department of Social Services manages mental healthcare. ↩
States that did not meet Pew’s criteria for a healthcare quality monitoring system were: Alaska, Connecticut, Delaware, Hawaii, Iowa, Montana, North Carolina, North Dakota, Oregon, Rhode Island, Virginia, and West Virginia. ↩
Alabama, Kansas, and New Hampshire did not respond to Pew’s survey. ↩
Twenty-eight states have some form of state-level oversight of minimum standards, including Department of Corrections oversight (15 states), independent commissions (7 states), Sheriff’s associations (4 states), and Department of Health oversight (2 states). Meanwhile, 21 states have no clearly defined mechanism in place to evaluate the safety of jails. See table 4 in Deitch’s report for a more detailed list of statewide jail oversight bodies by state as of March 2020. ↩
Deitch found that minimum standards tend not to cover entire substantive areas like use of force, and usually cannot evaluate how jails are handling issues not covered by their standards, meaning a lot of aspects of incarceration that impact health and safety can easily escape scrutiny. ↩
While inspections are most often mandatory, in some places they are voluntary. ↩
Often the consequence for failing to meet standards is censure (or a formal expression of disapproval), but sometimes departments can face financial penalties for noncompliance. ↩
According to Deitch’s findings:
- Staffing varies widely, from one staff person to scores of employees dedicated to oversight in some capacity. Some have the authority and duty to conduct routine inspections, while others can only respond to individual complaints and don’t have inspection responsibilities.
- 15 states and Washington, D.C. have independent mechanisms for responding to complaints and assessing and reporting on conditions.
- Three of the oversight bodies are non-governmental organizations that have legal authority or informal arrangements to physically access prisons.
- Two states have oversight bodies that only handle a discrete subset of issues.
- One state has a citizens’ advisory panel.
It’s worth noting that accreditation was measured as the number of accredited individual staff who became certified through the National Commission on Correctional Healthcare, not facilities. It’s understandable why the researchers used this as a measurement given the absence of facility-level mortality or litigation data, but it nonetheless places a limitation on the research. ↩
Oversight agencies tend to have the ability to make recommendations but usually can’t force departments to take action. ↩
To meet the “deliberate indifference” to “serious medical needs” standard under Estelle, the indifference must be the result of specific policies rather than individual choices. What constitutes a “serious medical need” depends on the discretion of the corrections department; if that department determined at the time that the medical need was not serious, then they could not be “deliberately indifferent” to it. In other words, corrections actors must have engaged in deliberate indifference after recognizing that the medical needs were serious. As Headworth and Zaborenko explain, courts typically don’t treat failures to meet basic competence standards, or failure to recognize or identify medical needs as “serious,” as evidence of legal wrongdoing, so the failure to identify problems becomes vindication, not liability. ↩
While better care outcomes may reduce emergency healthcare spending, the goal here is not a preoccupation with savings but rather the fulfillment of incarcerated peoples healthcare needs. In other words, reduced emergency spending may be offset or exceeded by other forms of healthcare spending on incarcerated people when they are actually receiving the care they need — care that is frequently altered, delayed, or denied under the current system. ↩
This dissertation by Margaret Lynn Charleroy at the University of Minnesota gives a detailed example of healthcare at the penitentiary in Minnesota, which saw its medical program expand rapidly between the 1880s and early 1900s. ↩
While there is limited information on this practice, it appears to have been bad enough that the National Commission on Correctional Health Care (NCCHC) felt compelled to issue a position statement in 2000 against hiring medical personnel with restricted licenses. “State licensing boards should not issue licenses that restrict licensed health care professionals’ employment solely to correctional environments,” they wrote, adding that “NCCHC and [the Society of Correctional Physicians] believe that such practice imparts a sense that patients in a correctional environment are undeserving of qualified care that is similar to care available in the community. This concept is anathema to the important medical canons of ethics and disregards the important public health role correctional health care can play.” ↩
The rise in total correctional spending was likely due to the growth of overall prison populations in the states. Meanwhile, the per-person spending rate was likely influenced by the healthcare needs and characteristics of the population, such as the aging of the population, substance use, mental illness, and the spread of infectious disease. ↩
Smaller jails with whiter populations were more likely to be served by local healthcare providers, whereas larger jails with greater non-white populations tended to contract with private companies. By population, corporations provided medical care to more than 20% of New York state’s local jail population but in New York City, 90% received care from a corporation. ↩
Table 1 has a detailed table on the breakdown by state. New Hampshire did not provide data. ↩
Some services (like mental health treatment) may be outsourced at specific facilities but the bulk of services were managed and provided by the state (hence “majority”). ↩
Colorado, Louisiana, Michigan, Minnesota, Montana, Pennsylvania, Rhode Island, and Virginia. ↩
Connecticut, Georgia, New Jersey, and Texas. ↩
About the author
Brian Nam-Sonenstein is a Senior Editor and Researcher at the Prison Policy Initiative. He is the author of several publications, including a report analyzing how prison disciplinary policies are used as a tool for mass punishment, as well as briefings explaining why ending mass incarceration is an economic justice issue and how providing housing can help interrupt a major pathway to prison created by the criminalization of homelessness. In addition to his work as a researcher, Brian plays a pivotal role in supporting other members of the Research Department in shaping the framing and messaging of their publications in a way that maximizes their impact and reach.
About the Prison Policy Initiative
The non-profit, non-partisan Prison Policy Initiative was founded in 2001 to expose the broader harm of mass criminalization and spark advocacy campaigns to create a more just society. The organization is known for its visual breakdown of mass incarceration in the U.S., as well as for its campaigns against prison gerrymandering and the predatory prison and jail telephone industry. The organization sounded the alarm in 2020 on the danger of COVID-19 outbreaks in prisons and jails, and continues to produce research on health topics including HIV prevalence in prisons and the high mortality rates of people under correctional control.
Acknowledgments
All Prison Policy Initiative reports are collaborative endeavors, and this report is no different. The authors would particularly like to thank current staff members for their insights and guidance. We would like to extend our gratitude to Bryant Jackson-Green of UC Irvine for providing the initial data on medical consent decrees, as well as the Prisoners Legal Advocacy Network (PLAN) for legal analysis as it relates to correctional healthcare. We would also like to thank the dozens of incarcerated people who responded to our inquiries and shared their experiences with prison healthcare systems. Lastly, we would like to thank our donors who make this work possible.
Events
- April 15-17, 2025:
Sarah Staudt, our Director of Policy and Advocacy, will be attending the MacArthur Safety and Justice Challenge Network Meeting from April 15-17 in Chicago. Drop her a line if you’d like to meet up!
Not near you?
Invite us to your city, college or organization.